Trends in Clinical and Medical Sciences
ISSN: 2791-0814 (online) 2791-0806 (Print)
DOI: 10.30538/psrp-tmcs2021.0004
A prospective study to evaluate accuracy of urine albumin-creatinine ratio in diagnosis of pre-eclampsia; A single centre observational study
Ataur Kamal Rashid, Mozafar Khazaei\(^1\)
Department of Obstetrics & Gynaecology, University of Medical Science & Technology, Khartoum, Sudan.; (A.K.R & M.K)
\(^{1}\)Corresponding Author: mkhazaei1345@yahoo.com
Abstract
Keywords:
1. Introduction
Pre-eclampsia (PE) is defined as a pregnancy-specific syndrome of reduced organ perfusion secondary to vasospasm and endothelial dysfunction. It is considered to be major reason for maternal mortality. It forms 12-20% of pregnancy related deaths [1] The number of cases in developing countries is on rise and it is approximately 4-19%. Pre- existing cardiovascular diseases (CVDs) may increase the prevalence of Pre-eclampsia (PE) in females [2,3].
The diagnosis of Pre-eclampsia is made with the presence of proteinuria > 300 mg /24hours and occurrence of blood pressure is at or >140/90 mmHg occurring on two occasions at least at interval of six hours [4]. Severe forms of preeclampsia can be complicated by renal, cardiac, pulmonary, hepatic, and neurological dysfunction; hematologic disturbances; fetal growth restriction; stillbirth; and maternal death [5]. It is regarded as hypertensive disorders of pregnancy. There are few risk factors for Pre-eclampsia such as obesity with BMI >30, diabetes mellitus, maternal age >35 years, chronic hypertension, chronic kidney disease (CKD), obstructive sleep apnea, pregestational diabetes, systemic lupus erythematosus (SLE) etc [6].
The pathogenesis of Pre-eclampsia occurs in two stages. The first stage consists of defective invasion of the deciduas by the fetal trophoblasts along with local placental hypoxia [7]. The second stage is characterized by liberation of placental blood-related components into the maternal circulation and aberrant expression of angiogenic, anti-angiogenic and pro-inflammatory factors [8]. The important factor is albumin which play an important role in diagnosis [9]. Patients with Pre-eclampsia shows microalbuminuria hypothesizing that the gross proteinuria stage is followed by the microalbuminuria stage. This test needs to wait for atleast 24 hours. Alternative methods to this method are dipstick and spot urinary protein: creatinine ratio, urine albumin-creatinine ratio.10 Considering this, the present study was attempted to determine cases of pre-eclampsia with spot urine albumin-creatinine ratio (ACR).
2. Methodology
This single centre, prospective study was conducted following approval from Review and ethical committee of the centre. One hundred ten pregnancies within 20-28 weeks of gestation were included in our study.A detailed clinical history and physical examination was conducted. Informed written consent was obtained from study patients. Parameters such as age, BMI, parity, gestational age at delivery, mode of delivery, birth weight of neonates etc. was recorded. Subjects were routinely evaluated for blood pressure measurement and all clinical features of pre-eclampsia were recorded. Spot mid- stream urine sample was collected from all pregnant females and urine ACR estimation was done using immunoturbidimetric microalbumin method and modified Jaffe's method for creatinine estimation. Results of study were recorded and subjected for statistical inferences using Mann Whitney U test. The level of significance was significant if p value is below 0.05.
3. Results
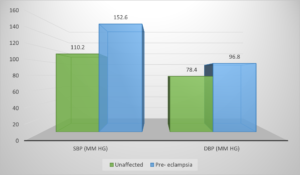
The distribution of patients based on blood pressure parameters is given in Table 1. Significance is < 0.05, Mann Whitney U Systolic blood pressure (SBP) in unaffected subjects was 110.2 mm Hg and in pre- eclamplsia was 152.6 mm Hg. Diastolic blood pressure (DBP) in unaffected subjects was 78.4 mm Hg and in pre- eclamplsia was 96.8 mm Hg. Mann Whitney U test showed significant difference between two (\(P< 0.05\)) (Significant, Table 1, Figure 1).
Table 1. Distribution of patients based on blood pressure parameters.
| Variables | Unaffected | Pre- eclampsia | P value |
|---|---|---|---|
| SBP (mm Hg) | 110.2 | 152.6 | <0.05 |
| DBP (mm Hg) | 78.4 | 96.8 | <0.05 |
Figure 1. Graphic representation of the effect of ICT Solutions on total anthropogepainic GHG supply
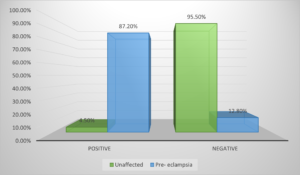
In unaffected subjects, 4.5% showed positive test and 95.5% showed negative test. In pre- eclampsia subjects, 87.2% showed positive test and 12.8% showed negative test. Mann Whitney U test showed significant difference between two (Significant, \(P< 0.05\)) (Table 2, Figure 2).
Table 2. Association of preeclampsia with UACR.
| UACR | Unaffected | Pre- eclampsia | P value |
|---|---|---|---|
| Positive | 4.5% | 87.2% | 0.05 |
| Negative | 95.5% | 12.8% | |
| Total | 100% | 100% |
Figure 2. Graphic representation of the effect of ICT Solutions on total anthropogepainic GHG supply
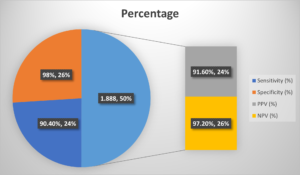
A sensitivity of 90.4%, specificity of 98%, PPV of 91.6% and NPV of 97.2% was seen (Table 3, Figure 3).
Table 3. Accuracy of UACR.
| Variables | Percentage | |
|---|---|---|
| Sensitivity (%) | 90.4% | |
| Specificity (%) | 98% | |
| PPV (%) | 91.6% | |
| NPV (%) | 97.2% | |
Figure 3. Graphic representation of the effect of ICT Solutions on total anthropogepainic GHG supply
4. Discussion
This is a single centre, observation study on one hundred ten pregnant females with gestation between 20-28 weeks. Numerous research projects are in existing literature mentioning utility of urine albumin-creatinine ratio (ACR) for the diagnosis of Pre-eclampsia. In our centre, we attempted to evaluate cases of Pre-eclampsia using albumin-creatinine ratio (ACR). Preeclampsia is defined as new-onset hypertension and new-onset end-organ damage. The pathophysiology of Preeclampsia comprises of multiple organ systems [11]. The situation starts with invasion of abnormal trophoblast before clinical features of the disease become apparent. During normal implantation, trophoblasts invade the decidualized endometrium, resulting in spiral artery remodeling and obliteration of the tunica media of myometrial spiral arteries, permitting raised blood flow to the placenta, all independent of maternal vasomotor changes [12]. It is apparent that in preeclampsia, trophoblasts fail to adopt an endothelial phenotype leading to altered trophoblast invasion and incomplete spiral artery remodeling [13].Our study showed that systolic blood pressure was 110.2 mm Hg in unaffected subjects and 152.6 mm Hg in pre- eclamplsia. Diastolic blood pressure was 78.4 mm Hg in unaffected subjects and 96.8 mm Hg in pre- eclamplsia. A study by Mahajan et al., [14]. validated the accuracy of the spot urine ratio of albumin-creatinine in asymptomatic pregnant women comprising of 150 patients. Results demonstrated that 28 patients had high ACR value, 2.4% (3) remained normotensive while 89.3% (25) had pre-eclampsia. It was further observed that among 81.3% (122) patients that were ACR negative, 10.7% (3) patients developed pre-eclampsia. A higher sensitivity of 89.29%, specificity 97.54%, positive predictive value (PPV) of 89.29% and the negative predictive value (NPV) of 97.54% was observed with urine albumin-creatinine ratio.
We noted that 4.5% showed positive test and 95.5% showed negative test in unaffected subjects. 87.2% showed positive test and 12.8% showed negative test in pre- eclampsia subjects. We found that most of the subjects who showed UACR positive had pre-eclampsia and only few subjects remained unaffected. Sachan et al., [15] in their study evaluated the diagnostic accuracy of albumin-creatinine ratio (ACR) in woman with preeclampsia and eclampsia and examine the association between ACR and fetomaternal outcome in 30 preeclampsia (cases), 30 antepartum eclampsia (cases) and 30 normotensive pregnant women (controls). The mean urinary ACR value was \(0.103 ± 0.037\) which was significantly lower than controls. On comparing between groups, the difference was significant (\(< 0.001\)), a strong correlation between urinary ACR levels and 24 hours urinary proteins was observed.
Renal dysfunction in preeclampsia is defined as serum creatinine >1.1 mg/dl or a doubling of baseline creatinine. Renal blood flow and glomerular filtration rate are often decreased in preeclampsia [16]. Biopsy changes in these patients include diffuse fibrin deposition, endothelial swelling, loss of podocytes, and loss of capillary space (glomerular endotheliosis). Dysregulation of the glomerular filtration apparatus occurs in the setting of glomerular endotheliosis [17]. In normal pregnancy, increased tissue factor release from the maternal decidua and placenta shifts endothelial cells to a procoagulant balance. Increased pro-inflammatory cytokines in preeclampsia further stimulate tissue factor expression by endothelial cells and leukocytes [18].
The definitive treatment for preeclampsia is delivery. American College of Obstetricians and Gynecologists has recommended daily aspirin intake. The United States Preventive Services Task Force and the International Society for the Study of Hypertension in Pregnancy also recommended delivery to be the option for high-risk women after 12 weeks gestation to reduce their risk of preeclampsia [19]. Aspirin is proposed to reduce preeclampsia risk via inhibition of cyclooxygenase-1 and cyclooxygenase-2, which contribute to prostaglandin biosynthesis and subsequent endothelial dysfunction. A study by Devi et al., [20] on 400 ladies were assessed at first booking visit at 18-20 weeks. The mean age of the patients was \(20.5±0.5\) and \(24.5±0.5\) years. It was observed that the spot UACR may be a simple, convenient, and accurate indicator of significant proteinuria and future complications in women with preeclampsia with proper and intensive clinical follow up and intervention to prevent feto maternal morbidity and mortality.
Conclusion
The role of urine albumin creatinine ration in detection of Pre-eclampsia is evident. A higher sensitivity and specificity revealed its usefulness in early detection.Author Contributions
All authors contributed equally to the writing of this paper. All authors read and approved the final manuscript.Conflicts of Interest
The authors declare no conflict of interest.References
- Gaziano, T. A., Bitton, A., Anand, S., Abrahams-Gessel, S., & Murphy, A. (2010). Growing epidemic of coronary heart disease in low-and middle-income countries. Current Problems in Cardiology, 35(2), 72-115. [Google Scholor]
- Nkoke, C., & Luchuo, E. B. (2016). Coronary heart disease in sub-Saharan Africa: still rare, misdiagnosed or underdiagnosed?. Cardiovascular Diagnosis and Therapy, 6(1), 64-66. [Google Scholor]
- Ebireri, J., Aderemi, A. V., Omoregbe, N., & Adeloye, D. (2016). Interventions addressing risk factors of ischaemic heart disease in sub-Saharan Africa: a systematic review. BMJ Open, 6(7), e011881. [Google Scholor]
- Mensah, G. A. (2008). Ischaemic heart disease in Africa. Heart, 94(7), 836-843. [Google Scholor]
- Makubi, A., Hage, C., Lwakatare, J., Kisenge, P., Makani, J., Rydén, L., & Lund, L. H. (2014). Contemporary aetiology, clinical characteristics and prognosis of adults with heart failure observed in a tertiary hospital in Tanzania: the prospective Tanzania Heart Failure (TaHeF) study. Heart, 100(16), 1235-1241. [Google Scholor]
- Haines, A., Patterson, D., Rayner, M., & Hyland, K. (1992). Prevention of cardiovascular disease. Occasional paper (Royal College of General Practitioners), (58), 67-78. [Google Scholor]
- Neter, J. E., Stam, B. E., Kok, F. J., Grobbee, D. E., & Geleijnse, J. M. (2003). Influence of weight reduction on blood pressure: a meta-analysis of randomized controlled trials. Hypertension, 42(5), 878-884.[Google Scholor]
- O'donnell, M. J., Mente, A., Smyth, A., & Yusuf, S. (2013). Salt intake and cardiovascular disease: why are the data inconsistent?. European Heart Journal, 34(14), 1034-1040. [Google Scholor]
- Parikh, S. V., & De Lemos, J. A. (2006). Biomarkers in cardiovascular disease: integrating pathophysiology into clinical practice. The American Journal of the Medical Sciences, 332(4), 186-197. [Google Scholor]
- Wang, J., Tan, G. J., Han, L. N., Bai, Y. Y., He, M., & Liu, H. B. (2017). Novel biomarkers for cardiovascular risk prediction. Journal of Geriatric Cardiology, 14(2), 135-150. [Google Scholor]
- Ridker, P. M., Hennekens, C. H., Buring, J. E., & Rifai, N. (2000). C-reactive protein and other markers of inflammation in the prediction of cardiovascular disease in women. New England Journal of Medicine, 342(12), 836-843. [Google Scholor]
- Joshi, P., Islam, S., Pais, P., Reddy, S., Dorairaj, P., Kazmi, K., ... & Yusuf, S. (2007). Risk factors for early myocardial infarction in South Asians compared with individuals in other countries. JAMA, 297(3), 286-294. [Google Scholor]
- Dwivedi, S., Anupam, P., & Chathurvedi, A. (1997). Cardiovascular risk factor in young coronary artery heart disease patient around East Delhi. South Asian Journal of Preventive Cardiol, 1, 21-26. [Google Scholor]
- Panwar, R. B., Gupta, R., Gupta, B. K., Raja, S., Vaishnav, J., Khatri, M., & Agrawal, A. (2011). Atherothrombotic risk factors & premature coronary heart disease in India: a case-control study. The Indian Journal of Medical Research, 134(1), 26-32. [Google Scholor]
- Enas, E. A., Yusuf, S., & Mehta, J. (1996). Meeting of the international working group on coronary artery disease in South Asians. 24 March 1996, Orlando, Florida, USA. Indian Heart Journal, 48(6), 727-732.[Google Scholor]
- Low, P. S., Heng, C. K., Saha, N., & Tay, J. S. H. (1996). Racial variation of cord plasma lipoprotein (a) levels in relation to coronary risk level: a study in three ethnic groups in Singapore. Pediatric Research, 40(5), 718-722. [Google Scholor]
- Roman, W. P., Martin, H. D., & Nkya, E. S. (2019). Assessment of risk factors for cardiovascular diseases among patients attending cardiac clinic at a referral hospital in Tanzania. Journal of Xiangya Medicine, 4, Article No. 18. [Google Scholor]
- Hasan, A., Agarwal, A., & Anjum Parvez, M. A. S. (2013). Premature coronary artery disease and risk factors in India. Indian Journal of Cardiology, 16, (1-2), 5-11. [Google Scholor]
- Hossain, A., & Khan, H. T. (2007). Risk factors of coronary heart disease. Indian heart journal, 59(2), 147-151. [Google Scholor]
- Kannel, W. B. (2009). Hypertension: reflections on risks and prognostication. Medical Clinics of North America, 93(3), 541-558. [Google Scholor]