Trends in Clinical and Medical Sciences
ISSN: 2791-0814 (online) 2791-0806 (Print)
DOI: 10.30538/psrp-tmcs2021.0010
Outcome of 82 cases of nasal polyposis undergoing functional endoscopic sinus surgery
Ankush Sathiyan, Hari Mahajan Jain, Sarfaraz Alam Khan\(^1\)
Department of Surgery, Manipala Institute of Medical Sciences, Pokharan, Nepal.; (A.S & H.M.J & S.A.K)
\(^{1}\)Corresponding Author: drsarfarazalamkhan1@gmail.com
Abstract
Keywords:
1. Introduction
Nasal polyposis is chronic inflammatory disease nasal mucosa and of sinus resulting in oedematous polyp protruding in nasal cavity [1]. It is also known as chronic rhinosinusitis with nasal polyps (CRSwNP) [2]. The striking feature of nasal polyposis is nasal discharge, congestion, nasal blockage and obstruction [3]. There is reduction or complete loss of smell in patients suffering from nasal polyposis. The presence of 2 or more symptoms are sufficient to make diagnosis. Endoscopy shows presence of polyps and mucopurulent discharge from the middle meatus or oedema, mucosal obstruction primarily in the middle meatus [4].
Chronic RS (CRS) is those which is present for longer duration of time. It may be divided into those in which nasal polyps are present and those in which they are absent [5]. A thorough clinical, histopathologic features and CT is useful in making diagnosis. CT scan of sinuses shows mucosal changes within the osteomeatal complex and/or sinuses. Interleukin profile is also necessary for the diagnosis [6].
Management of patients of nasal polyposis comprised of intranasal steroids. Patients taking systemic steroids shows improvement of air flow, reduction in polyp size and decrease recurrence of polyps [7]. In patients where symptomatic treatment with topical or systemic steroids fails, surgical management is regarded best treatment option and for patients with complications. Functional endoscopic sinus surgery (FESS) is one of the treatment options highly efficacious in relieving symptoms, improving sinus ventilation and drainage and for removing polyps [8]. Patients being treated for polyp disease derive the greatest benefit from functional endoscopic sinus surgery, and those whose main preoperative symptom is nasal obstruction or headache report higher benefit [9]. In this prospective observation study, we studied 82 cases of nasal polyposis undergoing functional endoscopic sinus surgery (FESS).
2. Methodology
This prospective observation study, a total of 82 patients presenting with the symptoms of nasal polyposis were studied. It comprised of 38 male patient and 44 female patients. Higher authorities' approval was sorted. A written informed consent was taken before starting this project. The inclusion criteria consisted of patients with nasal polyposis confirmed with CT, age above 18 years of either sex, absence of comorbidities, patients not responding to medicinal treatment.All patients were clinically evaluated with anterior rhinoscopy and nasal endoscopy was performed by otorhinolaryngologist pre and post operatively. FESS was performed following all aseptic standardized procedure. Parameters assessed were NOSE score and nasal endoscopy score. NOSE score comprised of recording of symptoms such as nasal congestion, nasal obstruction, trouble nasal breathing, trouble sleeping and unable to get enough air through nose during exercise and it is either not a problem, very mild problem, moderate problem, fairly bad problem and severe problem having score 0,1,2,3,4 respectively. Nasal endoscopy score comprised of factors such as polyp, discharge, oedema, scarring and crusting with score 0, 1 and 2. Results of study were recorded and subjected for statistical inferences using Mann Whitney U test. The level of significance was significant if p value is below 0.05.
3. Results
Age wise distribution of patients is presented in Table 1. Maximum patients were seen in age group 18-28 years ie 35 (42.6%), followed by 28-38 years 20 (24.3%), 38-48 years 15(18.2%), 48-58 years 7 (8.5%) and >58 years 5 (6%).
Table 1. Age wise distribution of patients.
| Age group | Number | Percentage |
|---|---|---|
| 18-28 years | 35 | 42.6 |
| 28-38 years | 20 | 24.3 |
| 38-48 years | 15 | 18.2 |
| 48-58 years | 7 | 8.5 |
| >58 years | 5 | 6 |
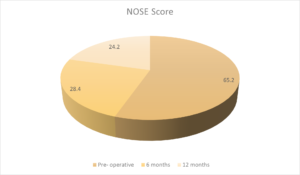
Significance, \(< 0.05\), Mann Whitney U Pre- operative NOSE score was \(65.2\pm 5.7\), at 6 months was \(28.4\pm 4.1\) and at 12 months post- operatively was \(24.2\pm 3.6\). Mann Whitney U test showed significant p value \(< 0.05\) (Table 2, Figure 1).
Table 2. NOSE score.
| Duration | Mean | SD | P value |
|---|---|---|---|
| Pre- operative | 65.2 | 5.7 | Significant, P< 0.05 |
| 6 months | 28.4 | 4.1 | |
| 12 months | 24.2 | 3.6 |
Figure 1. NOSE score
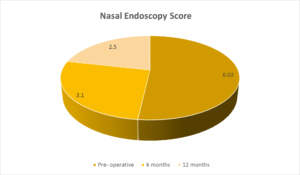
A pre- operative nasal endoscopic score was 6.02, 6 months score was 3.1 and 12 months score was 2.5. Mann Whitney U test showed significant with p value < 0.05 (Figure 2).
4. Discussion
We studied 82 cases of nasal polyposis undergoing functional endoscopic sinus surgery (FESS). Chronic rhinosinusitis (CRS) is a common health problem which leads to frequent visits to primary care physicians and ear, nose, throat specialists [10]. In spite of the recent advances, the etiology, pathogenesis and treatment of CRS is a matter of debate [11]. Nasal polyposis (NP) is considered as a subgroup of CRS with an incidence of 4% in general population and 25-30% in patients suffering from CRS. Nasal polyps (NP) are mucosal sacs containing oedema, fibrous tissue, vessels, inflammatory cells and glands [12]. Functional endoscopic sinus surgery (FESS) is the treatment of choice for CRS patients not responding to drug therapy. It is a multifactorial disease linked to bacterial infection, allergy, biofilms and recently superantigens. The symptom manifestation of CRS is varied [13]. Therefore, clinical assessment by major and minor criteria, assisted by nasal endoscopy and CT scan are the usual methods of diagnosis and management. The universal rationale of treatment is adequate drainage and aeration of the sinus [14].There were 38 male patient and 44 female patients. A study by Nair et al., [15] included 90 patients of nasal polyposis undergoing FESS. It was found in our study that maximum patients were seen in age group 18-28 years ie 35 (42.6%), followed by 28-38 years 20 (24.3%), 38-48 years 15(18.2%), 48-58 years 7 (8.5%) and >58 years 5 (6%). Nair et al., [15] study on 38 patients of chronic rhinosinusitis and 52 patients of nasal polyps showed that patients of nasal polyp group presented with increased severity of symptoms of nasal blockage, nasal discharge and reduced sense of smell as compared to the chronic rhinosinusitis group who had significantly higher presentation of headache and facial pain. The preoperative CT scan revealed significantly higher bilateral disease with increased involvement of multiple sinuses in nasal polyp group. Post endoscopic sinus surgery both the groups showed significant improvement in their symptoms with the nasal polyp group demonstrating reduction in improvement on 1 year follow up.
Pre- operative NOSE score was \(65.2\pm 5.7\), at 6 months was \(28.4\pm 4.1\) and at 12 months post- operatively was \(24.2\pm 3.6\). A study by Kayat et al., [16] on 50 patients diagnosed with nasal polyposis underwent recoding of Lund-Mackay CT scan score, pre-operative nasal endoscopy score and pre-operative NOSE score followed by post- operative score recording at 6 months and 12 months. Both NOSE score and Nasal Endoscopy Score showed statistically significant improvement between Pre-operative and Post-operative 6 months score. However no statistically significant improvement between post- operative 6 months score and post-operative 12 months score. The Pre-operative CT Scan score had poorly positive correlation with Pre-operative Nasal Endoscopy Score. The Pre-operative Nasal Endoscopy Score correlated negatively with Preoperative NOSE score.
A pre- operative nasal endoscopic score in our patients was 6.02, 6 months score was 3.1 and 12 months score was 2.5. Kenny et al., [17] correlated smell sense with radiological findings only and found it significant. Significant correlation of olfactory scores with each of CT, endoscopic, and subjective scores both before and 3 months after sinus surgery. Ryan et al., [18] correlated symptomatology, endoscopic, and radiological criteria in CRS patients and found poor correlation but found subjective impaired sense of smell to be correlating closely with abnormal endoscopic findings. Rosbe et al., [19] studied whether symptoms and endoscopic grade could be predicted by CT scan. For patients with objective findings on imaging and endoscopy, nasal obstruction and postnasal drainage were the most likely to correlate, and headache and facial pain were the least likely.
Wang et al., [20] undertook study of surgical outcomes of functional endoscopic sinus surgery and radical sinus surgery for refractory rhinosinusitis on 56 cases with refractory rhinosinusitis which were classified into functional endoscopic surgery group (FESS group) and radical sinus surgery group (RSS group). On comparison of age, gender, complicated with allergic rhinitis and asthma, no significant difference between two groups was observed (P> 0.05). However, there was significant difference between two groups in the number of patients with previous surgery (P< 0.05). Pre-operative VAS symptom score, Lund-Kennedy score and Lund-Mackay score were higher in RSS group than in FESS group. VAS symptom score (P< 0.01), Lund-Kennedy score (P< 0.01), Lund-Mackay score (P< 0.01) were significantly lower after surgery. There was no significant difference in VAS symptom scores between two groups postoperatively (P> 0.05). However, Lund-Kennedy score (P< 0.01) and Lund-Mackay score (P< 0.01) were lower in RSS group postoperatively. Among patients with surgery history, Lund-Kennedy score (P< 0.01) and Lund-Mackay score (P< 0.01) were also lower in RSS group at one year follow-up.
5. Conclusion
Functional endoscopic sinus surgery is treatment of choice in patients with chronic rhinosinusitis with nasal polyps. Patients Endoscopy Score and NOSE symptom score was improved after treatment.Author Contributions
All authors contributed equally to the writing of this paper. All authors read and approved the final manuscript.Conflicts of Interest
The author declares no conflict of interest.References
- Kaplan, B. A., & Kountakis, S. E. (2004). Role of nasal endoscopy in patients undergoing endoscopic sinus surgery. American Journal of Rhinology, 18(3), 161-164. [Google Scholor]
- Stankiewicz, J. A., & Chow, J. M. (2002). Nasal endoscopy and the definition and diagnosis of chronic rhinosinusitis. Otolaryngology—Head and Neck Surgery, 126(6), 623-627. [Google Scholor]
- Andrews, P. J., Poirrier, A. L., Lund, V. J., & Choi, D. (2016). Outcomes in endoscopic sinus surgery: olfaction, nose scale and quality of life in a prospective cohort study. Clinical Otolaryngology, 41(6), 798-803. [Google Scholor]
- Gupta, D., Gulati, A., Singh, I., & Tekur, U. (2014). Endoscopic, radiological, and symptom correlation of olfactory dysfunction in pre-and postsurgical patients of chronic rhinosinusitis. Chemical Senses, 39(8), 705-710. [Google Scholor]
- Bradley, D. T., & Kountakis, S. E. (2005). Correlation between computed tomography scores and symptomatic improvement after endoscopic sinus surgery. The Laryngoscope, 115(3), 466-469. [Google Scholor]
- Kennedy, D. W. (1992). Prognostic factors, outcomes and staging in ethmoid sinus surgery. The Laryngoscope, 102(12 Pt 2 Suppl 57), 1-18. [Google Scholor]
- Robinson, J. L., Griest, S., James, K. E., & Smith, T. L. (2007). Impact of aspirin intolerance on outcomes of sinus surgery. The Laryngoscope, 117(5), 825-830. [Google Scholor]
- Linder, J. A., & Atlas, S. J. (2004). Health-related quality of life in patients with sinusitis. Current Allergy and Asthma Reports, 4(6), 490-495. [Google Scholor]
- Armstrong, M. (2005). Office-based procedures in rhinosinusitis. Otolaryngologic Clinics of North America, 38(6), 1327-1338. [Google Scholor]
- Smith, T. L., Batra, P. S., Seiden, A. M., & Hannley, M. (2005). Evidence supporting endoscopic sinus surgery in the management of adult chronic rhinosinusitis: a systematic review. American Journal of Rhinology, 19(6), 537-543. [Google Scholor]
- Ling, F. T., & Kountakis, S. E. (2007). Important clinical symptoms in patients undergoing functional endoscopic sinus surgery for chronic rhinosinusitis. The Laryngoscope, 117(6), 1090-1093. [Google Scholor]
- Bhattacharyya, N. (2004). Symptom outcomes after endoscopic sinus surgery for chronic rhinosinusitis. Archives of Otolaryngology–Head & Neck Surgery, 130(3), 329-333. [Google Scholor]
- Osguthorpe, J. D. (2001). Adult rhinosinusitis: diagnosis and management. American Family Physician, 63(1), 69-76. [Google Scholor]
- Fokkens, W. J., Lund, V. J., & Mullol, J. (2007). European position paper on rhinosinusitis and nasal polyps 2007: A summary for otorhinolaryngologists. Rhinology, 45(2), 97-101. [Google Scholor]
- Nair, S., Dutta, A., Rajagopalan, R., & Nambiar, S. (2011). Endoscopic sinus surgery in chronic rhinosinusitis and nasal polyposis: a comparative study. Indian Journal of Otolaryngology and Head & Neck Surgery, 63(1), 50-55. [Google Scholor]
- Kayet, B., Ghosh, P., & Sengupta, A. (2019). Subjective and objective assessment of outcome in Nasal polyposis after functional endoscopic sinus surgery. Journal of Medical Science and Clinical Research, 7(6), 1080-1085. [Google Scholor]
- Kenny, T. J., Duncavage, J., Bracikowski, J., Yildirim, A., Murray, J. J., & Tanner, S. B. (2001). Prospective analysis of sinus symptoms and correlation with paranasal computed tomography scan. Otolaryngology—Head and Neck Surgery, 125(1), 40-43. [Google Scholor]
- Ryan, W. R., Ramachandra, T., & Hwang, P. H. (2011). Correlations between symptoms, nasal endoscopy, and in-office computed tomography in post-surgical chronic rhinosinusitis patients. The Laryngoscope, 121(3), 674-678. [Google Scholor]
- Rosbe, K. W., & Jones, K. R. (1998). Usefulness of patient symptoms and nasal endoscopy in the diagnosis of chronic sinusitis. American Journal of Rhinology, 12(3), 167-172. [Google Scholor]
- Wang, M. J., Lin, F., Zhang, X. Q., Zhou, B., Cui, S. J., & Li, Y. C. (2017). Analysis of surgical outcomes of functional endoscopic sinus surgery and radical sinus surgery for refractory rhinosinusitis. Journal of Clinical Otorhinolaryngology, Head, and Neck Surgery, 31(3), 185-190. [Google Scholor]