Trends in Clinical and Medical Sciences
ISSN: 2791-0814 (online) 2791-0806 (Print)
DOI: 10.30538/psrp-tmcs2021.0006
Topical triamcinolone acetonide, oral methotrexate, and a combination of topical triamcinolone acetonide and oral methotrexate in the management of oral lichen planus- A comparative study
Raj Srivastava\(^1\), Arjun Kapoor, Sachin Mehta, Amit Chauhan
Department of Pharmacology, Rajendra Institute of Medical Sciences & Research Centre, Gangtok, Sikkim, India.; (R.S & A.K & S.M & A.C)
\(^{1}\)Corresponding Author: rkshrivastava.dean@gmail.com
Abstract
Keywords:
1. Introduction
Lichen planus is frequently occurring muco- cutaneous disease. It is one of the auto-immune inflammatory disease which has high impact on mental health of life. It is commonly occurring in females and middle age group is leading affected group [1]. It occurs in various forms such as reticular, bullous, erosive, erythematous, plaque, annular, papular etc [2,3,4]. It is one of the potentially malignant disorder in where chances of conversion to oral cancer is high [5]. Erosive form has high malignant potential [6]. The most striking oral feature of oral lichen planus is the presence of wickham striations. These are radiating greyish whitish striations commonly occur in buccal mucosa [7]. Other sites involved are lips, gingiva, soft palate etc. The predisposing factor for lichen planus is stress, depression, anxiety, psychiatric disorders [8].
Various treatment options are available for the management of lichen planus such as use of topical, systemic steroids, immunomodulators, herbal products etc [9]. Triamcinolone acetonide is one of the topical corticosteroids found to be effective in the management of oral lichen planus. Topical steroids is preferred over systemic steroids owing to its less side effects [10,11]. Methotrexate is one of the immunosuppressant drug inhibiting dihydrofolate reductase competitively, therefore hinder replication and function of T and B lymphocytes [12]. Its efficacy against cutaneous, oral erosive and vulvovaginal LP found be high [13]. Few studies have demonstrated equal effect of corticosteroids and methotrexate in oral lichen planus cases [14,15,16]. Considering this, this study was undertaken with the aim to compare 0.1% topical triamcinolone acetonide, oral methotrexate, and a combination of 0.1% topical triamcinolone acetonide and oral methotrexate in the management of oral lichen planus.
2. Methodology
This prospective, observation, comparative study was commenced with the permission of ethical clearance committee of the institute. It has 60 cases (males- 20, females- 40). Inclusion criteria used was occurrence of moderate to severe LP, age group 18-60 years, biopsy approved cases and those giving consent. Exclusion criteria was cases not in specified age group and those having contraindication to v methotrexate.A computer-generated randomization of patients was done into 3 groups. Group T was given 0.1% topical triamcinolone acetonide, group M was given topical methotrexate and group C was given combination of both 0.1% topical triamcinolone acetonide and oral methotrexate. 0.1% topical triamcinolone acetonide was prescribed three times daily and methotrexate 0.3 mg/kg once/week. Patients were advised to continue the treatment for 4 months. Remission was defined absence of signs and symptoms of lesions. Live function test and complete blood count was determined. Clinical severity score was also calculated. The objective improvement was graded as excellent, good, poor, no response and worsening. Visual analog scale (VAS) was used for pain assessment. Results of the present study after recording all relevant data were subjected for statistical inferences using chi- square test. The level of significance was significant if p value is below 0.05 and highly significant if it is less than 0.01.
3. Results
Group T had 3.2 years, group M had 3.1 years and group C had 3.3 years of duration of symptoms. A non- significant difference between groups was observed (P> 0.05) (Table 1).
Table 1. Comparison of symptoms.
| Parameters | Group T | Group M | Group C | P value |
|---|---|---|---|---|
| Duration of symptoms (years) | 3.2 | 3.1 | 3.3 | >0.05 |
| Difficulty in eating and/or drinking (%) | 85% | 90% | 94% | >0.05 |
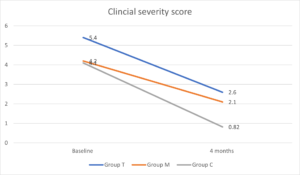
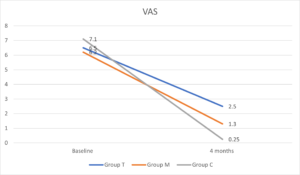
It was observed that mean CSS at baseline was 5.4 in group T, 4.2 in group M and 4.1 in group C and at 4 months was 2.6 in group T, 2.1 in group M and 0.82 in group C. Baseline VAS was 6.5 in group T, 6.2 in group M and 7.1 in group C and at 4 months was 2.5 in group T, 1.3 in group M and 0.25 in group C. A significant difference between groups was observed (P< 0.05) (Table 2, Figures 1 and 2).
Table 2. Comparison of CSS and VAS in all groups.
| Parameters | Group T | Group M | Group C | P value |
|---|---|---|---|---|
| Baseline CSS | 5.4 | 4.2 | 4.1 | >0.05 |
| 4 months CSS | 2.6 | 2.1 | 0.82 | >0.05 |
| Baseline VAS | 6.5 | 6.2 | 7.1 | >0.05 |
| 4 months VAS | 2.5 | 1.3 | 0.25 | >0.05 |
Figure 1. Clinical severity score
Figure 2. VAS
4. Discussion
This was an observational study attempted to compare different treatment modalities in oral lichen planus patients. We involved 60 patients which were randomly divided equally 3 groups of 20 each based on treatment option adopted. The result of our study showed that Group T had 3.2 years, group M had 3.1 years and group C had 3.3 years of duration of symptoms. Chauhan et al., [17] evaluated the clinical efficacy and safety of topical triamcinolone 0.1% oral paste, oral methotrexate and a combination of these in symptomatic moderate-to severe OLP. Forty-five patients were recruited and were allocated to three treatment arms. It was observed that all three treatment modalities were effective. The patients in the combination group had significantly better reduction in the outcome parameters assessed compared to the other two groups. 9 patients observed complete clinical remission, 6 in the combination group and 3 in the topical triamcinolone group. Systemic methotrexate, alone or in combination with topical triamcinolone, is effective in management of moderate to severe OLP.It was observed in our study that mean CSS at baseline was 5.4 in group T, 4.2 in group M and 4.1 in group C and at 4 months was 2.6 in group T, 2.1 in group M and 0.82 in group C. Baseline VAS was 6.5 in group T, 6.2 in group M and 7.1 in group C and at 4 months was 2.5 in group T, 1.3 in group M and 0.25 in group C. Malhotra et al., [18] involved 49 patients with moderate to severe oral lichen planus. Group A patients received either OMP comprising 5 mg of betamethasone orally on 2 consecutive days per week, group B received triamcinolone acetonide (0.1%) paste application thrice daily for 3 months. 23 of 25 patients in group A and 23 of 24 patients in group B completed the study. Good to excellent response was seen in 17 of 25 (68.0%) patients in group A as compared with 16 of 24 (66.0%) in group B at 6 months. Symptom-free state was achieved in 13 of 25 (52%) patients in group A and 12 of 24 (50%) in group B. The difference in the mean scores within each group was statistically significant from the fourth week onward in group A and eighth week onward in group B, whereas in patients with erosive disease it was second and twelfth week onward, respectively. Chamani et al., [19] compared effects of tacrolimus, clobetasol, and pimecrolimus on OLP and found that there was insufficient evidence to support superior efficacy of any specific treatment out of these three agents.
In our study in group C, combination of methotrexate and topical triamcinolone was significantly better than the other groups. This better result can be presumed to be due to the synergistic anti-inflammatory effects of methotrexate and triamcinolone as they seem to suppress inflammation via different pathways. Another advantage of this combination could be that topical corticosteroids help to reduce the dose of systemic therapy.
The term lichen planus was termed by Wilson in 1869. Cutaneous lesions typically present as small (2 mm) pruritic, white to violaceous flat-topped papules, which can increase in size to as much as 3 cm. Lichen planus patient usually manifests with burning sensation in oral cavity, the eating, speaking and drinking become difficult. Extreme painful condition make patient weak as ingestion become difficult. Reticular lichen planus is most common form occurs in 60-65% of cases. The interlacing striations give rise of red dot called stria of Wickham. Biopsy of the lesion reveal presence of colloid bodies, civatte bodies and hyaline bodies. Basal cell degeneration and saw tooth rete pegs are characteristic features [20]. The differential diagnosis should include lichenoid reactions, leukoplakia, squamous cell carcinoma, pemphigus, mucous membrane pemphigoid, and candidiasis. Lichenoid reactions in the oral cavity are invariably drug-induced lesions. The erosive or atrophic types that affect the gingiva should be differentiated from pemphigoid, as both may have a desquamative clinical appearance. Lupus erythematosus often has white plaque-like lesions with an erythematous border. In some cases, erythema multiforme can resemble bullous lichen planus, but it is more acute and generally involves the labial mucosa [21].
5. Conclusion
The result of our study showed that combination of triamcinolone and methotrexate exhibited maximum relieve of symptoms in patients with oral lichen planus.Author Contributions
All authors contributed equally to the writing of this paper. All authors read and approved the final manuscript.Conflicts of Interest
The authors declare no conflict of interest.References
- Adamo, D., Ruoppo, E., Leuci, S., Aria, M., Amato, M., & Mignogna, M. D. (2015). Sleep disturbances, anxiety and depression in patients with oral lichen planus: a case–control study. Journal of the European Academy of Dermatology and Venereology, 29(2), 291-297. [Google Scholor]
- Chamani, G., Rad, M., Zarei, M. R., Lotfi, S., Sadeghi, M., & Ahmadi, Z. (2015). Efficacy of tacrolimus and clobetasol in the treatment of oral lichen planus: a systematic review and meta-analysis. International Journal of Dermatology, 54(9), 996-1004. [Google Scholor]
- Duong, B., Marks, S., Sami, N., & Theos, A. (2012). Lichen planus pemphigoides in a 2-year-old girl: response to treatment with methotrexate. Journal of the American Academy of Dermatology, 67(4), e154-e156. [Google Scholor]
- Farhi, D., & Dupin, N. (2010). Pathophysiology, etiologic factors, and clinical management of oral lichen planus, part I: facts and controversies. Clinics in Dermatology, 28(1), 100-108.[Google Scholor]
- Hazra, S. C., Choudhury, A. M., Khondker, L., & Khan, S. I. (2013). Comparative efficacy of methotrexate and mini pulse betamethasone in the treatment of lichen planus. Mymensingh Medical Journal, 22(4), 787-797. [Google Scholor]
- Ivanovski, K., Nakova, M., Warburton, G., Pesevska, S., Filipovska, A., Nares, S., ... & Angelov, N. (2005). Psychological profile in oral lichen planus. Journal of Clinical Periodontology, 32(10), 1034-1040. [Google Scholor]
- Jang, N., & Fischer, G. (2008). Treatment of erosive vulvovaginal lichen planus with methotrexate. Australasian Journal of Dermatology, 49(4), 216-219. [Google Scholor]
- Slade, G. D. (1997). Derivation and validation of a short-form oral health impact profile. Community Dentistry and Oral Epidemiology, 25(4), 284-290. [Google Scholor]
- Sugerman, P. B., Satterwhite, K., & Bigby, M. (2000). Autocytotoxic T-cell clones in lichen planus. British Journal of Dermatology, 142(3), 449-456. [Google Scholor]
- Torti, D. C., Jorizzo, J. L., & McCarty, M. A. (2007). Oral lichen planus: a case series with emphasis on therapy. Archives of Dermatology, 143(4), 511-515. [Google Scholor]
- Turan, H., Baskan, E. B., Tunali, S., Yazici, S., & Saricaoglu, H. (2009). Methotrexate for the treatment of generalized lichen planus. Journal of the American Academy of Dermatology, 60(1), 164-166. [Google Scholor]
- Ismail, S. B., Kumar, S. K., & Zain, R. B. (2007). Oral lichen planus and lichenoid reactions: etiopathogenesis, diagnosis, management and malignant transformation. Journal of Oral Science, 49(2), 89-106. [Google Scholor]
- Zakrzewska, J. M., Chan, E. Y., & Thornhill, M. H. (2005). A systematic review of placebo-controlled randomized clinical trials of treatments used in oral lichen planus. British Journal of Dermatology, 153(2), 336-341. [Google Scholor]
- Shengyuan, L., Songpo, Y., Wen, W., Wenjing, T., Haitao, Z., & Binyou, W. (2009). Hepatitis C virus and lichen planus: a reciprocal association determined by a meta-analysis. Archives of Dermatology, 145(9), 1040-1047. [Google Scholor]
- Harman, M., Akdeniz, S., Dursun, M., Akpolat, N., & Atmaca, S. (2004). Lichen planus and hepatitis C virus infection: an epidemiologic study. International Journal of Clinical Practice, 58(12), 1118-1119. [Google Scholor]
- Usatine, R. P., Smith, M. A., Mayeaux, E. J., & Chumley, H. S. (Eds.). (2009). The Color Atlas of Family Medicine. McGraw-Hill Medical. [Google Scholor]
- Chauhan, P., De, D., Handa, S., Narang, T., & Saikia, U. N. (2018). A prospective observational study to compare efficacy of topical triamcinolone acetonide 0.1% oral paste, oral methotrexate, and a combination of topical triamcinolone acetonide 0.1% and oral methotrexate in moderate to severe oral lichen planus. Dermatologic Therapy, 31(1), e12563. [Google Scholor]
- Malhotra, A. K., Khaitan, B. K., Sethuraman, G., & Sharma, V. K. (2008). Betamethasone oral mini-pulse therapy compared with topical triamcinolone acetonide (0.1%) paste in oral lichen planus: A randomized comparative study. Journal of the American Academy of Dermatology, 58(4), 596-602. [Google Scholor]
- Chamani, G., Rad, M., Zarei, M. R., Lotfi, S., Sadeghi, M., & Ahmadi, Z. (2015). Efficacy of tacrolimus and clobetasol in the treatment of oral lichen planus: a systematic review and meta-analysis. International Journal of Dermatology, 54(9), 996-1004. [Google Scholor]
- Eisen, D. (1999). The evaluation of cutaneous, genital, scalp, nail, esophageal, and ocular involvement in patients with oral lichen planus. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology, 88(4), 431-436. [Google Scholor]
- Dissemond, J. (2004). Oral lichen planus: an overview. Journal of Dermatological Treatment, 15(3), 136-140. [Google Scholor]