Trends in Clinical and Medical Sciences
ISSN: 2791-0814 (online) 2791-0806 (Print)
DOI: 10.30538/psrp-tmcs2022.0025
Assessment of traumatic axial cervical spine injuries
Sarvar Akbarov Alisherovich
Director of private medical clinic Med Elite, Center for the Development of professional Qualifications of Medical workers, Tashkent, Uzbekistan.; urolog.sarvar@gmail.com
Abstract
Methodology: Eighty-four patients with traumatic axial cervical spine injuries of either gender were enrolled. Magnetic imaging resonance (MRI) was performed in all. Conservative treatment was given to those with minimal no bony injuries with or without spinal cord contusion, and decompression and fixation were performed in moderate to severe bony injuries with spinal cord compression. In addition, patients were treated for anterior fixation, i.e., corpectomy with either autologous bone graft or titanium cage and plate fixation and with corpectomy with tricorticate graft.
Results: Out of 84 patients, males comprised 54 (64.2\%), and females had 30 (35.8\%). Aetiology in the present found to be assault in 9, road traffic accident in 48, sports injury in 17, and workplace injury in 10 cases. Body fracture was evident in 24 and ligamentous injury in 60 patients. The type of body fractures was C3 in 3, C4 in 2, C5 in 12, C6 in 3, and C7 in 4 patients. Management performed was corpectomy with tricorticate graft in 26 cases and a corpectomy with fixation with a titanium cage and plate/screws in 58 cases.
Conclusion: Discoligamentous was a major type of injury, and road traffic accident was the main cause of injury among patients with subaxial cervical spine injuries.
Keywords:
1. Introduction
Subaxial cervical spine injuries carry high mortality and morbidity. These comprise facet joint fractures and disruption of joint capsule [1]. Subaxial cervical spine injuries involve either anterior column injuries such as those involving body fractures, middle column injuries such as facets injuries, or posterior column injuries such as laminar injuries and posterior osteoligamentous injuries [2]. In the case of anterior column injuries, compression and comminuted fracture injuries of the vertebral body are common [3]. It is indicated when there is evidence of spinal canal compression resulting from a fractured segment breaching into the spinal canal [4]. Correction of the kyphotic deformity occurred due to wedge fracture. Posterior column injuries comprise injuries of the lamina and various ligaments [5,6].
Various treatment modalities have emerged over the period of time regarding the treatment of traumatic axial cervical spine injuries. Both anterior and posterior approaches with the help of autologous and synthetic bone grafts for fixation have been tried by Neurosurgeons [7,8]. There is variation in the management of traumatic subaxial cervical spine injuries. Stabilization of facet joint either by immobilization or fixation of levels above and below the level of fracture is the main treatment option [9].
Considering this, we attempted present a retrospective, observational study to assess traumatic axial cervical spine injuries in 84 patients.
2. Methodology
A sum total of eighty- four patients with traumatic axial cervical spine injuries of either gender. They became part of the study with their written consent. Ethical clearance was obtained from the review and clearance committee.The demographic profile of each patient was entered in the case history proforma. All cases were managed in casualty with primary resuscitation with trauma protocol and spine immobilization. They underwent clinical and radiological investigations. Magnetic imaging resonance (MRI) was performed in all. Conservative treatment was given to those with minimal no bony injuries with or without spinal cord contusion, and decompression and fixation were performed in moderate to severe bony injuries with spinal cord compression. Patients were treated for anterior fixation, i.e., corpectomy with either autologous bone graft or a titanium cage and plate fixation and with corpectomy with tricorticate graft. Results were compiled and spread along an MS excel sheet for correct inference. SPSS version 18.0 with Chi-square test was performed for comparison with the level of significance set below 0.05.
3. Results
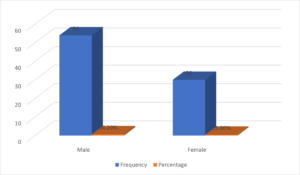
Out of 84 patients, males comprised 54 (64.2%) and females had 30 (35.8%) (Table 1, Figure 1).
Table 1. Patients distribution.
| Gender | Frequency | Percentage |
|---|---|---|
| Male | 54 | 64.2% |
| Female | 30 | 35.8% |
Figure 1. Graph I Patients distribution.
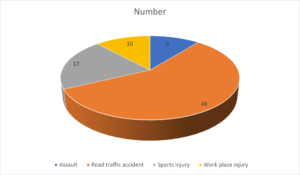
Aetiology in present found to be assault in 9, road traffic accident in 48, sports injury in 17 and work place injury in 10 cases. A significant difference was observed (P< 0.05) (Table 2, Figure 2).
Table 2. Aetiology of injury.
| Aetiology | Number | P value |
|---|---|---|
| Assault | 9 | <0.05 |
| Road traffic accident | 48 | |
| Sports injury | 17 | |
| Work place injury | 10 |
Figure 2. Graph II Aetiology of injury.
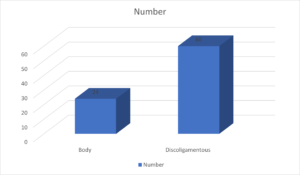
Body fracture was evident in 24 and ligamentous injury in 60 patients. The difference found to be significant (P< 0.05) (Table 3, Figure 3).
Table 3. Type of injury noted in patients.
| Type of injury | Number | P value |
|---|---|---|
| Body | 24 | <0.05 |
| Discoligamentous | 60 |
Figure 3. Graph III Type of injury noted in patients.
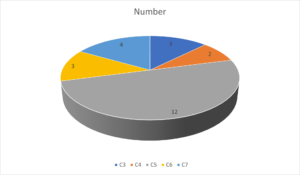
Type of body fractures was C3 in 3, C4 in 2, C5 in 12, C6 in 3 and C7 in 4 patients. The difference found to be significant (P< 0.05) (Table 4, Figure 4).
Table 4. Type of body fractures.
| Body fractures | Number | P value |
|---|---|---|
| C3 | 3 | <0.05 |
| C4 | 2 | |
| C5 | 12 | |
| C6 | 3 | |
| C7 | 4 |
Figure 4. Graph IV Type of body fractures.
Management performed was corpectomy with tricorticate graft in 26 cases and corpectomy with fixation with titanium cage and plate/screws in 58 cases. The difference was significant (P< 0.05) (Table 5).
Table 5. Management performed in cases.
| Management | Number | P value |
|---|---|---|
| Corpectomy with tricorticate graft | 26 | 0.05 |
| Corpectomy with fixation with titanium cage and plate/screws | 58 |
4. Discussion
Spinal cord injuries (SCIs) are a major cause of disability and mortality in the modern world [10]. Cervical spine injuries occur in 2% to 3% of all blunt trauma [11,12]. The permanent disability and lack of societal and vocational integration associated with SCI make it a burden on the patient and the family [13,14]. Since quadriplegia or quadriparesis resulting from cervical spine injuries cause significant disability, it becomes more critical to promptly manage these injuries in the hope of a better functional recovery [15,16]. The retrospective observational study assessed traumatic axial cervical spine injuries in 84 patients. Out of 84 patients, males comprised 54 (64.2%) and females had 30 (35.8%).Aetiology in the present found to be assault in 9, road traffic accident in 48, sports injury in 17, and workplace injury in 10 cases. Dhakal et al., [17] in their study, 30 subaxial cervical trauma patients were divided into four groups based on the timing of surgery: within two days, 3 to 7 days, 8 to 30 days, and >31 days. There were 27 male and three female patients. Forty-four had an injury due to a fall. No patients were treated within the first 48 hours; only nine were treated between 3 and 7 days, 16 between 8 and 30 days, and five a month later. The major delay was finance and operating room availability. Thirteen patients had a C6C7 involvement, followed by C5C6 in 6 patients. Seven patients had complete neurological deficit, while 18 patients had an incomplete deficit. A total of 46.7% improved their neurology in 6 months. No neurological recovery was observed in complete deficit patients.
Our results showed that body fracture was evident in 24 and ligamentous injury in 60 patients. Type of body fractures was C3 in 3, C4 in 2, C5 in 12, C6 in 3, and C7 in 4 patients. Ulrich et al., [18]. Coe et al., [19] tested several implants in cadaver and bovine spines. They concluded that the posterior approach is far better than the anterior one, especially in associated ligamental injuries. Ulrich et al., [18] said an additional external immobilization should be combined with anterior fixation, whereas Coe et al., [19] recommended posterior wiring techniques.
Management performed was corpectomy with tricorticate graft in 26 cases and a corpectomy with fixation with a titanium cage and plate/screws in 58 cases. Venkati et al., [20] conducted a study on 172 patients with subaxial cervical spine injuries, of which 44 patients suffered from vertebral body fracture. In comparison, 108 patients had spinal canal compromise due to other injuries. Sixteen patients had quadriplegia, 24 had grade 4 power in upper and lower extremities, and roots were involved in 46 patients. In 44 patients complete corpectomy was performed with the placement of a tricorticate graft taken from the fibula. This graft was fixed in place with a titanium plate and four screws.
Asher et al., [21] conducted a study on 452 patients, of which 69.7% were males, and 30.3% were females. 52.4% patients were between the age group 30-60 years of age, and about 56.1% had hospital stays lasting < 10 days. 46.6% of patients exhibited road traffic accidents as the primary common mechanism of injury. Neck pain was the most common symptom, and cervical spine straightening was the most common radiological abnormality. The injuries were more severe in patients who were not restrained by a seat belt or wearing a helmet.
The shortcoming of the present study is that a small sample size was included. In addition, we did not include those who died during the treatment.
5. Conclusion
Discoligamentouswas major type of injury and road traffic accident was main cause of injury among patients with subaxial cervical spine injuries.Author Contributions:
All authors contributed equally to the writing of this paper. All authors read and approved the final manuscript.Conflicts of Interest:
''The authors declare no conflicts of interest.''References
- Bohlman, H. H. (1979). Acute fractures and dislocations of the cervical spine. An analysis of three hundred hospitalized patients and review of the literature. JBJS, 61(8), 1119-1142. [Google Scholor]
- Capen, D. A., Garland, D. E., & Waters, R. L. (1985). Surgical stabilization of the cervical spine. A comparative analysis of anterior and posterior spine fusions. Clinical Orthopaedics and Related Research, 196, 229-237. [Google Scholor]
- Coe, J. D., Warden, K. E., Sutterlin III, C. E., & McAFEE, P. C. (1989). Biomechanical evaluation of cervical spinal stabilization methods in a human cadaveric model. Spine, 14(10), 1122-1131. [Google Scholor]
- Argenson, C., Lovet, J., Sanouiller, J. L., & De Peretti, F. (1988). Traumatic rotatory displacement of the lower cervical spine. Spine, 13(7), 767-773. [Google Scholor]
- Bombard, M., & Canevet, D. (1984). Comparison over the entire series of the results of anterior and posterior surgery. Revue de Chirurgie Orthopedique et Reparatrice, 70, 533-536. [Google Scholor]
- de Oliveira, J. C. (1979). Anterior reduction of interlocking facets in the lower cervical spine. Spine, 4(3), 195-202. [Google Scholor]
- Stauffer, E. S., & Kelly, E. G. (1977). Fracture-dislocations of the cervical spine. The Journal of Bone and Joint Surgery, 59(1), 45-48. [Google Scholor]
- Castaing, J. (1984). Prior surgical treatment in recent trauma to the lower cervical spine. Revue de Chirurgie Orthopedique et Reparatrice, 70, 519-522. [Google Scholor]
- Castaing, J. (1984). Arguments in favor of the anterior approach in traumatic chinirgia of the cervical spine. Revue de Chirurgie Orthopedique et Reparatrice, 70, 556-557. [Google Scholor]
- Reid, D. C., Henderson, R., Saboe, L., & Miller, J. D. (1987). Etiology and clinical course of missed spine fractures. The Journal of Trauma, 27(9), 980-986. [Google Scholor]
- McCleary, A. J. (1993). A fracture of the odontoid process complicated by tenth and twelfth cranial nerve palsies: A case report. Spine, 18(7), 932-935. [Google Scholor]
- Arias, M. J. (1985). Bilateral traumatic abducens nerve palsy without skull fracture and with cervical soine fracture: case report and review of the literature. Neurosurgery, 16(2), 232-234. [Google Scholor]
- Stiell, I. G., Clement, C. M., McKnight, R. D., Brison, R., Schull, M. J., Rowe, B. H., ... & Wells, G. A. (2003). The Canadian C-spine rule versus the NEXUS low-risk criteria in patients with trauma. New England Journal of Medicine, 349(26), 2510-2518. [Google Scholor]
- Yadollahi, M., Paydar, S., Ghaem, H., Ghorbani, M., Mousavi, S. M., Akerdi, A. T., ... & Bolandparvaz, S. (2016). Epidemiology of cervical spine fractures. Trauma Monthly, 21(3), Article ID, e33608, https://doi.org/10.5812/traumamon.33608. [Google Scholor]
- Fredo, H. L., Rizvi, S. A. M., Lied, B., Ronning, P., & Helseth, E. (2012). The epidemiology of traumatic cervical spine fractures: a prospective population study from Norway. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine, 20, Article No. 85. https://doi.org/10.1186/1757-7241-20-85. [Google Scholor]
- Kiwerski, J., Weiss, M., & Chrostowska, T. (1981). Analysis of mortality of patients after cervical spine trauma. Spinal Cord, 19(6), 347-351. [Google Scholor]
- Dhakal, G. R., Bhandari, R., Dhungana, S., Poudel, S., Gurung, G., Kawaguchi, Y., & Riew, K. D. (2019). Review of subaxial cervical spine injuries presenting to a tertiary-level hospital in Nepal: challenges in surgical management in a third world scenario. Global Spine Journal, 9(7), 713-716. [Google Scholor]
- Ulrich, C., Wörsdörfer, O., Claes, L., & Magerl, F. (1987). Comparative study of the stability of anterior and posterior cervical spine fixation procedures. Archives of Orthopaedic and Traumatic Surgery, 106(4), 226-231. [Google Scholor]
- Roy-Camille, R. (1984). Arguments in favor of the posterior approach in traumatic cervical spine surgery. Revue de Chirurgie Orthopedique et Reparatrice, 70, 550-557. [Google Scholor]
- Venkati, G. S., Satpaty, A., Pandey N.,& Prasad, R. S. (2021). Observational retrospective study of subaxial cervical spine trauma at tertiary care centre. IP Indian Journal of Neurosciences, 7(4),306-310. [Google Scholor]
- Asher, P., Joseph, J. J., Pendro, V. S., Peethambaran, A., & Prabhakar, R. B. (2020). Epidemiological study of cervical spine injury in a tertiary care center in South India. International Surgery Journal, 7(9), 2895-2898. [Google Scholor]