Trends in Clinical and Medical Sciences
ISSN: 2791-0814 (online) 2791-0806 (Print)
DOI: 10.30538/psrp-tmcs2022.0024
Open and closed damage to the abdomen with associated trauma
Sobirjon Ergashevich Mamarajabov\(^{1}\), Ishnazar Boynazarovich Mustafakulov\(^{2}\) and Zilola Aramovna Djurayeva\(^{3}\)
\(^{1}\) Head of the Department of Operative Surgery and Topographic Anatomy of Samarkand State Medical University, Dean of the Faculty of International Education, Ph.D.; Samarkand, Uzbekistan.
\(^{2}\) Docent., Head of the department of surgical diseases, Samarkand, Uzbekistan.
\(^{3}\) Lecturer of the Department of Endocrinology, Samarkand, Uzbekistan.
Correspondence should be addressed to Sobirjon Ergashevich Mamarajabov at m_sobirjon@yahoo.com
Abstract
Keywords:
1. Introduction
Abdominal injuries account for 1.5 to 36.5% of peacetime injuries, but their frequency and severity continue to increase. According to A.N. Tulupov[1,2], in severe concomitant trauma, injuries to the abdominal organs are present in almost 30% of victims. Due to the severity of damage to internal organs and difficulties in diagnosis, such an injury is characterized by a high rate of complications and mortality, which, according to various authors, ranges from 25 to 65%. According to Shapot [3,4] and Afonina [5], with an isolated injury of one abdominal cavity, the lethality ranges from 5.1 to 20.4%, and with a combined injury - from 18.3 to 64% [6,7,8,9,10,11,12,13].
Closed abdominal injuries are accompanied by a large number of complications and high mortality due to difficulties in diagnosis and frequent combination with injuries to other organs, and systems [14,15,16,17,18,19,20,21]. A particular problem is the diagnosis and treatment of concomitant closed trauma of the abdominal organs, accompanied by shock. Hospital mortality in this variant of the pathology ranges from 17.3 to 72.7% [22,23,24,25,26]. For example, over the past five years, the mortality rate from road accidents in Russia has increased by 65%, and the death toll reaches 33-35 thousand people per year [27,28,29].
In the literature, several terms define multiple injuries to various areas of the body in severe trauma [30,31]. In the Russian literature, the term severe concomitant injury (TTS) is most often used. However, in the big medical encyclopedia [32] there is the following definition: polytrauma - simultaneous damage to several anatomical areas in one victim.
Concomitant injuries are simultaneous damage to several different systems or organs. TCT as a model of an extreme condition, is damage to two or more anatomical regions of the body. Concomitant injury, defined as the simultaneous injury of two or more of the body's seven anatomical regions, is a complex multifactorial and severe type of injury characterized by numerous pathological syndromes, a frequent change in the dominant factor, a large number of complications, and a high mortality rate. In the diagnosis, the authors recommend indicating the leading injury. Thus, the analysis of scientific literature indicates that the choice of the volume of surgical intervention in patients with severe concomitant abdominal trauma against the background of traumatic and hemorrhagic shock is still an unsolved problem [33,34,35].
The purpose of the study
Improvement of the results of surgical treatment of damage to the abdominal organs in concomitant trauma by improving and introducing new methods of diagnosis and rational surgical tactics, depending on the severity of the injury.Materials and methods
Treatment of victims with severe concomitant abdominal injuries was carried out in the conditions of round-the-clock emergency surgical care in the Samarkand branch of the RSCEMP.For the period from 2009-2019. Two thousand six hundred forty-five patients with concomitant trauma of the abdominal cavity and retroperitoneal space were admitted to the Samarkand branch of the RSCEMP, of which 447 (16.9%) patients were operated on with concomitant abdominal trauma.
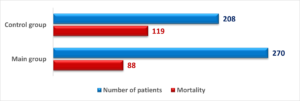
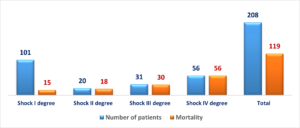
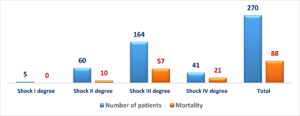
Our study consisted of two stages - a retrospective one based on the results of studying the case histories of 208 patients with shock-related mechanical trauma and a prospective one based on analyzing the treatment results of 270 critically ill patients hospitalized with concomitant trauma.
The criteria for inclusion in the research were the following attitudes: 1) shock-related concomitant mechanical trauma to the abdominal organs; 2) the age of the victims is from 18 to 89 years. The exclusion criteria were: 1) clinically significant comorbidities (oncological diseases and chronic diseases in the decompensated stage at the time of admission); 2) combined trauma of severe degree.
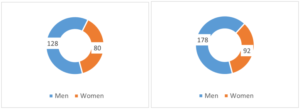
The study included 478 patients aged 18 to 89 years, among them - 306 men (64.0%) and 172 women (36.0%) - Figure 1.
Figure 1. Distribution of victims by gender.
Sorting of victims with abdominal injuries in cases of combined trauma by gender in the control and main groups is illustrated in Figure 2.
Figure 2. Distribution of victims by age of the control and main groups.
The average age of hospitalized patients was 33.8 \(\pm\) 13.4 years, and most of them were people of working age, which also emphasizes the relevance of the problem under study (Figure 3).
Figure 3. Distribution of victims by age.
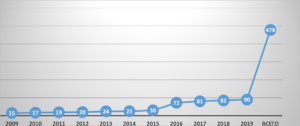
As seen in Figure 5, over ten years, the number of victims hospitalized in the SFRNCEMP increased six times. The overwhelming majority were delivered by ambulance teams - 416 (87%), who were provided with appropriate assistance at the scene of the accident to maintain the body's vital functions and prevent the development of life-threatening conditions. However, 62 victims (13%) were admitted by gravity without providing the necessary assistance (Figure 4)
Figure 4. Dynamics of admission of victims with concomitant injury
Figure 5. Ways of hospitalization of victims with associated trauma.
Among 478 victims, 447 (93.5%) were operated on. Of these, a lethal outcome was observed in the control group - out of 208 in 119 (57.21%), and in the main group - out of 270 - 88 (32.59%) - Figure 6. Thirty-one (11.48%) patients with abdominal injuries (liver in 25 and spleen in 6) underwent conservative therapy in the presence of concomitant injury.
Figure 6. Mortality in the study and control groups.
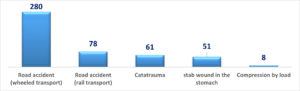
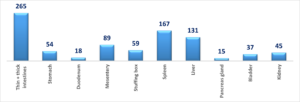
In most cases, the cause of injury was a road traffic accident (n = 358 - 74.89%), in 51 (10.67%) victims, the cause of injury was the result of striking the abdomen, in 61 (12.76%) catatrauma (Figure 7).
Figure 7. Distribution of patients by type and mechanism of injury.
Alcohol intoxication was observed in 257 (53.77%) victims.
The severity of shock was assessed using the Algover-Gruber index (shock index).
Sorting of victims according to the degree of hemorrhagic shock is presented in Table 1. The data in the table indicate that 478 (100%) patients undergoing examination were admitted in a state of hemorrhagic shock (I, II, III and IV degrees).
Table 2. Sorting of victims with concomitant trauma of the abdominal organs according to the severity of hemorrhagic shock upon admission.
| Index Algovera-Gruber | Shock degrees | Number of victims, n = 478 | Total died | ||
|---|---|---|---|---|---|
| I gr. | II gr. | I gr. | II gr. | ||
| Up to 1.0 | I | 101 | 5 | 15 | - |
| 1.0 to 1.5 | II | 20 | 60 | 18 | 10 |
| 1.5 to 2.0 | III | 31 | 164 | 30 | 57 |
| 2.1 and more | IV | 56 | 41 | 56 | 21 |
| Total | 208 | 270 | 119(57.21%) | 88(32.59%) | |
Figure 8. Dependence of the mortality rate on the degree of shock in the control group, n = 208.
Attention should be paid to the fact that in the control group, even with the development of hemorrhagic shock of the 1st degree, there were cases of lethal outcome; with the development of hemorrhagic shock of II, III, and IV degrees, almost 100% mortality was noted (Figure 8).
Figure 9. Dependence of the mortality rate on the degree of shock in the main group, n = 270.
With the use of improved surgical tactics in the leading group, lethality significantly decreased, with no lethal outcome in the case of grade I hemorrhagic shock, and 49% of patients with grade IV shock survived (Figure 9).
The following Figure 10 shows the terms of hospitalization of the victims in the hospital from the moment of injury. Most of the patients were hospitalized for 3 hours from the moment of injury (n = 292, 61.1%). Moreover, in the first hour after the injury - only 60 (12.55%) patients.
Figure 10. Distribution of victims by hospitalization period.
We also analyzed the frequency of damage to various anatomical areas of the body in victims with associated trauma (Figure 11). The largest group consisted of injuries to the head and limbs (62.0% and 58.9%, respectively), injuries to the chest organs - 40.5%, the spine - 27.2%, the pelvic bones, and urogenital organs - 22.9%, abdominal cavity - 21.2%.
Figure 11. Frequency of damage to various anatomical areas.
Among 478 patients with concomitant abdominal trauma, in 261 cases (54.6%), the predominant injury was abdominal trauma, in 131 cases (27.4%) - craniocerebral (TBI), in 60 patients (12.5%) - chest trauma and combined injuries were found in 26 (5.5%) cases.
Most often, abdominal injuries were associated with TBI and chest trauma (n = 271; 56.7% of cases).
It is important to note that in 94.1% of cases, injuries of two or more anatomical areas were detected.
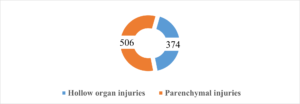
The total number of abdominal and retroperitoneal injuries detected in 478 patients is 880. Among the abdominal injuries, injuries of parenchymal organs were predominantly encountered (Figure 12).
Figure 12. The structure of abdominal injuries in victims.
Damage to the parenchymal organs (506) of the abdominal cavity and retroperitoneal space prevailed over injuries to the hollow organs (374) of the abdominal cavity (Figure 13).
Figure 13. Damage to the abdominal organs and retroperitoneal space with concomitant injury.
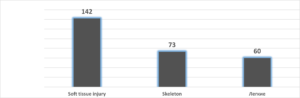
In addition, 275 patients had extra-abdominal injuries (Figure 14), which were characterized by damage to the skeleton, soft tissues and chest organs.
Figure 14. Extra-abdominal injuries in concomitant trauma.
2. Results and discussion
In these observations, we noted two prevailing syndromes: developing peritonitis syndrome and intra-abdominal bleeding syndrome. The syndrome of developing peritonitis was encountered with injuries to the hollow organs.The intra-abdominal bleeding syndrome was observed in the case of damage to the parenchymal organs or blood vessels of the mesentery and omentum, retroperitoneal space. At the same time, changes in hemodynamics were characteristic, as well as a decrease in several hematological parameters (hemoglobin, hematocrit, the number of erythrocytes), oliguria, and leukocytosis with the ruptured spleen (in 167).
We adhere to the following treatment tactics: with a distinct clinic for intra-abdominal bleeding and acute peritonitis - emergency operation (in 232 patients). In the absence of confidence in the presence of intra-abdominal bleeding and peritonitis, together with anti-shock therapy, such diagnostic methods are performed as pleural puncture (in 31), laparocentesis (in 40), laparoscopy (in 127), R-graph: skull (in 51), pelvis (in 30), spine (in 37), retrograde cystography (in 15), ultrasound (in 201) and computed tomography (in 40 patients).
The most common combined abdominal trauma was damage to the parenchymal organs in combination with damage to the intestine, bladder, and kidney. It is considered that trauma to the liver, spleen, kidney, and extensive retroperitoneal hematomas were more often observed with damage to the chest, pelvis, and spine. On admission, symptoms of internal bleeding were noted in 250 (52.3%) patients and 48 (10.0%) patients with symptoms of peritonitis.
3. Conclusion
The main cause of death among 478 patients was a combination of injuries in 127 victims (26.56%), as well as the development of complications. Among patients with injuries of the abdominal organs, they were observed in 80 (16.73%) in the postoperative period.Author Contributions:
All authors contributed equally to the writing of this paper. All authors read and approved the final manuscript.Conflicts of Interest:
''The authors declare no conflicts of interest.''References
- Paulino, J., Vigia, E., Cunha, M., & Amorim, E. (2020). Two-stage pancreatic head resection after previous damage control surgery in trauma: two rare case reports. BMC surgery, 20, Article No. 98. https://doi.org/10.1186/s12893-020-00763-2. [Google Scholor]
- Leijdesdorff, H. A., Gillissen, S., Schipper, I. B., & Krijnen, P. (2020). Injury pattern and injury severity of in-hospital deceased road traffic accident victims in the Netherlands: Dutch road traffic accidents fatalities. World Journal of Surgery, 44(5), 1470-1477. [Google Scholor]
- Cardi, M., Ibrahim, K., Alizai, S. W., Mohammad, H., Garatti, M., Rainone, A., ... & Sibio, S. (2019). Injury patterns and causes of death in 953 patients with penetrating abdominal war wounds in a civilian independent non-governmental organization hospital in Lashkargah, Afghanistan. World Journal of Emergency Surgery, 14, Article No. 51. https://doi.org/10.1186/s13017-019-0272-z. [Google Scholor]
- Valiev, E. Y. (2011). Experience in providing specialized care to patients with polytrauma in the conditions of the RSCEMP. collection. ''Modern military field surgery and surgery of injuries.'' St. Petersburg, 67-68. [Google Scholor]
- Pisano, M., Allievi, N., Gurusamy, K., Borzellino, G., Cimbanassi, S., Boerna, D., ... & Ansaloni, L. (2020). 2020 World Society of Emergency Surgery updated guidelines for the diagnosis and treatment of acute calculus cholecystitis. World Journal of Emergency Surgery, 15, Article No. 61. https://doi.org/10.1186/s13017-020-00336-x. [Google Scholor]
- Abdurakhmanovich, K. O., Zhavlanоvich, Y. D., Zairovna, A. U., Akmalovna, B. S., & Rakhmatullaevich, M. S. (2021). Possibilities of Sonography in Differential Diagnostics of Hematuria. Central Asian Journal of Medical and Natural Sciences, 2(4), 126-131. [Google Scholor]
- Shimizu, T., Umemura, T., Fujiwara, N., & Nakama, T. (2019). Review of pediatric abdominal trauma: operative and non-operative treatment in combined adult and pediatric trauma center. Acute Medicine & Surgery, 6(4), 358-364. [Google Scholor]
- Khan, M. (2018). Abdominal Trauma. InTrauma: Code Red (pp. 189-232). CRC Press. [Google Scholor]
- Lin, S., Wang, T. Y., Xu, H. R., Zhang, X. N., Wang, Q., Liu, R., ... & Bi, K. S. (2019). A systemic combined nontargeted and targeted LC-MS based metabolomic strategy of plasma and liver on pathology exploration of alpha-naphthylisothiocyanate induced cholestatic liver injury in mice. Journal of Pharmaceutical and Biomedical Analysis, 171, 180-192. [Google Scholor]
- Pulatovna, A. H. (2018). Prevalence and character of polytraumatic injuries among children population in Uzbekistan from 1995 to 2015. European Science Review, (1-2), 76-82. [Google Scholor]
- Alotaibi, F. A. A., Filimban, H. A., Almalki, R. S., Alsaman, A. A., Ahmed, W. M., Aldraihem, K. R., ... & Abood, H. B. A. (2021). Overview on Temporary Abdominal Closure Techniques: A Review. Journal of Pharmaceutical Research International, 68-74. [Google Scholor]
- Arlati, S. (2019). Pathophysiology of acute illness and injury. In Operative Techniques and Recent Advances in Acute Care and Emergency Surgery (pp. 11-42). Springer, Cham. [Google Scholor]
- Tulupov, A. N., Manukovskiy, V. A., Kazhanov, I. V., & Besaev, G. M. (2018). An experience in providing specialized medical care in closed combined injuries and injuries at the level i trauma center of saint-petersburg research institute of emergency medicine naii dzhanelidze. Medico-Biological and Socio-Psychological Problems of Safety in Emergency Situations, 25(2), 51-59. [Google Scholor]
- Gasques, D., Johnson, J. G., Sharkey, T., Feng, Y., Wang, R., Xu, Z. R., ... & Weibel, N. (2021, May). ARTEMIS: A collaborative mixed-reality system for immersive surgical telementoring. In Proceedings of the 2021 CHI Conference on Human Factors in Computing Systems (pp. 1-14). [Google Scholor]
- Mustafakulov, I. B., Shakirov, B. M., Elmuradov, A. N., Umedov, H. A., Normamatov, B. P., & Elmuradova, Z. A. (2022). The role of intra-abdominal pressure in injuries of the ab-dominal organs with associated injuries. International Journal of Surgery and Transplantation Research, 2(1), 1-3. [Google Scholor]
- Khadzhibaev, A. M., Rizaev, K. S., Riskiev, U. R., Shukurov, B. I., Yangiev, R. A., & Pulatov, M. M. U. (2021). Diagnosis and treatment of early intra-abdominal complications after cholecystectomy. Journal of Emergency Medicine , 14(5), 5-15. [Google Scholor]
- Khadjibaev, A. M., & Mirdjalilov, F. K. (2018). Quick diagnostics of fat embolism syndrome in patients with polytrauma. Vestnik Ekstrennoy Medisini. 2018(2), 19-23. [Google Scholor]
- Khadjibaev, F. A., Atadjanov, S. K., Karabaev, H. K., & Mustafaev, A. L. (2022). Results of treatment of closed pancreatic injuries in rscfema and its branches. Art of Medicine. International Medical Scientific Journal, 2(1), 138-148. [Google Scholor]
- Khadjibaev, A. M., & Sultanov, P. K. (2018). The algorithm of surgical treatment of patients with multiple trauma associated with falls from heights. Central Asian Journal of Medicine, 2018(2), 118-132. [Google Scholor]
- Khadjibaev, A. M., & Sultanov, P. K. (2018). Algorithm of surgical treatment for combined catatrauma. Herald of Tashkent Medical Academy, 2(30), 111-114. [Google Scholor]
- Safronov, D. (2019). Condition of the gastrointestinal tract motor function in abdominal injury. The Journal of VN Karazin Kharkiv National University, series ''Medicine'', 13(37), 56-61.[Google Scholor]
- Baghdanian, A., Baghdanian, A., Pham, T. H., & Steenburg, S. D. (2021). Imaging After Damage Control Surgery. In Atlas of Emergency Imaging from Head-to-Toe, (pp. 1-14). Cham: Springer International Publishing. [Google Scholor]
- Zargaran, D., Zargaran, A., & Khan, M. (2020). Systematic review of the management of retro-hepatic inferior vena cava injuries. Open Access Emergency Medicine: OAEM, 12, 163-171. [Google Scholor]
- Yang, X. Q., Ye, J., Li, X., Li, Q., & Song, Y. H. (2019). Pyrrolizidine alkaloids-induced hepatic sinusoidal obstruction syndrome: Pathogenesis, clinical manifestations, diagnosis, treatment, and outcomes. World Journal of Gastroenterology, 25(28), 3753-3763. [Google Scholor]
- Mustafakulov, I. B., & Umedov, K. A. (2022). Surgical tactics in case of isolated injuries of small and large intestine. Uzbek Medical Journal, 3(2), 1-12. [Google Scholor]
- Mustafakulov, I. B., Umedov, K. A., Karabaev, H. K., & Djuraeva, Z. A. (2021). Damage Control the Liver and Spleen in Case of Concomitant Injury (Literature Review). Advances in Clinical Medical Research, 2(2), 13-17.[Google Scholor]
- Mustafakulov, I. B., Elmuradov, A., Djuraeva, Z. A., & Umedov, H. A. (2021). Diagnostic tools and therapeutic possibilities of endovideolaparoscopy for combined abdominal trauma. Journal of Natural Remedies, 22(1(2)), 181-186. [Google Scholor]
- Mustafakulov, I. B., Tagaev, K. R., Muradova, R. R., Djuraeva, Z. A., & Sattorov, A. X. (2021). Results of treatment of patients with thermoingalation trauma. Journal of Natural Remedies, 22(1(2)), 187-195. [Google Scholor]
- Mustafakulov, I. B., & Djuraeva, Z. A. (2020). Severe associated trauma to the abdomen diagnosis and treatment. European Journal of Pharmaceutical and Medical Research, 7(6), 113-116. [Google Scholor]
- Mustafakulov, I. B. (2020). Severe combined abdominal trauma. Journal of Critical Reviews, 7(11), 2214-2221. [Google Scholor]
- Mustafakulov, I. B., & Djuraeva, Z. A. (2020). Evaluaton of the effectiveness of multi-stage surgical tactics for liver damage. World Journal of Advance Healthcare Research, 4(3), 264-266. [Google Scholor]
- Mustafakulov, I. B., & Djuraeva, Z. A. (2019). Intra-abdominal hypertension at combined injuries of the abdominal organs. American Journal of Medicine and Medical Sciences, 9(12), 499-502. [Google Scholor]
- Temirovich, A. M., Shonazarovich, S. I., Keldibaevich, A. G., Ismailovich, J. Z., Ugli, T. J., & Yashibayevich, S. Z. (2021). Prevention and treatment of intraabdominal hypertension in patients with peritonitis. Vestnik Nauki I Obrazovaniya, 2021(3-2(106)), 75-79. [Google Scholor]
- Abbasy, J. (2019). Experience of hydatid disease of liver at a tertiary care center 7 years experience. HPB, 21, S353-S354. [Google Scholor]
- Baker, J. E., Millar, D. A., Heh, V., Goodman, M. D., Pritts, T. A., & Janowak, C. F. (2020). Does chest wall Organ Injury Scale (OIS) or Abbreviated Injury Scale (AIS) predict outcomes? An analysis of 16,000 consecutive rib fractures. Surgery, 168(1), 198-204. [Google Scholor]