Trends in Clinical and Medical Sciences
ISSN: 2791-0814 (online) 2791-0806 (Print)
DOI: 10.30538/psrp-tmcs2022.0034
A clinico-pathological study of colonic biopsies
Alka Dixit Vats\(^{1}\) and Anubhav Garg(^{1,*}\)
\(^{1}\) Department of Pathology, Rama Medical College Hospital & Research Centre, Hapur, Uttar Pradesh, India.
Correspondence should be addressed to Anubhav Garg at dr.anubhavgarg@gmail.com
Abstract
Materials and methods: One hundred ten colonic biopsies obtained from Gastroenterology department were collected in 10% neutral buffered formalin processed and embedded with the mucosal surface being uppermost. 4\(\mu\) thick serial sections were prepared and stained with H&E. Detailed study of the sections was done under light microscope and diagnosis rendered accordingly.
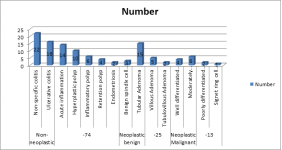
Result: Age group 11-20 years had 8, 21-30 years had 22, 31-40 years had 40, 41-50 years had 24 and >50 years had 16 cases. The difference was non- significant (\(P> 0.05\)). Most common clinical features were constipation seen in 36, bleeding PR in 28, bleeding PR weakness in 17, diarrhea in 16 and diarrhea \(+\) pain abdomen \(+\) weakness in 14 patients. The difference was non-significant (\(P> 0.05\)). Non-neoplastic lesions were 74. These were as non-specific colitis in 22, ulcerative colitis in 16, acute inflammation in 14, hyperplastic polyp in 10, inflammatory polyp in 6, retention polyp in 4 and endometriosis in 2 cases. Neoplastic benign lesions were 25. Benign spindle cell lesion was in 3, tubular adenoma in 15, villous adenoma in 5 and tubulovillous adenoma in 2 cases. Neoplastic malignant lesions were well differentiated adenocarcinoma seen in 4, moderately differentiated adenocarcinoma in 6, poorly differentiated adenocarcinoma in 2 and signet ring cell carcinoma in 1 case.
Conclusion: Colonoscopy is a simple and a safe procedure. It helps in assessing the lesions clinically and confirming histopathologicaly through guided biopsy. Colonoscopic biopsies also play a key role not only in diagnosis, but also in follow up and treatment.
Keywords:
1. Introduction
A variety of inflammatory and neoplastic disorders affect the lower gastrointestinal tract, with differing clinical outcomes and management. These conditions encompass a spectrum of acute and chronic conditions [1]. Colon is the primary site for various non neoplastic and neoplastic diseases. The spectrum of colonic lesions ranges from congenital diseases, infections, inflammatory conditions, vascular diseases, polyps and colorectal tumours. Colorectal carcinoma is one of the leading cause of morbidity and mortality with an overall cancer incidence rate of 9% [2].
The development of flexible endoscopes has led to the increase in the examination and mucosal biopsy evaluation of all portions of large intestine and rectum [3]. Another rapidly evolving technique is the Virtual colonoscopy, in which data from computed tomography are used to generate both two-dimensional and three-dimensional displays of the colon and rectum [4]. Vining introduced virtual colonoscopy in 1994 to maintain the desirable features of colonoscopy of ease of lesion detection while avoiding the undesirable features of colonoscopy of test invasiveness, patient discomfort, need for sedation, analgesia and test risks [5].
Colonic mucosal biopsies procured from colonoscopy plays a crucial role in specific diagnosis of patients with Inflammatory Bowel disease and early detection of colonic epithelial tumours. Histopathological interpretation of colonic mucosal biopsies when correlated with clinical finding helps in definitive diagnosis and early treatment of patients with colonic lesions [6]. Considering this, we performed clinico-pathological study of colonic biopsies.
2. Materials and methods
A sum total of one hundred ten colonic biopsies obtained from Gastroenterology department were selected for the study. Ethical clearance was obtained before starting the study. Inclusion criteria was all the colonoscopic biopsies taken from terminal ileum to rectum, received in the Department of Pathology. Exclusion criteria was poorly fixed/unfixed specimens.
After obtaining tissues, all colonoscopic biopsy specimens were collected in 10% neutral buffered formalin processed and embedded with the mucosal surface being uppermost. 4 \(\mu \) thick serial sections were prepared and stained with H &E. Detailed study of the sections was done under light microscope and diagnosis rendered accordingly. Results were tabulated and assessed statistically. P value less than 0.05 was considered significant.
3. Results
Age group 11-20 years had 8, 21-30 years had 22, 31-40 years had 40, 41-50 years had 24 and >50 years had 16 cases. The difference was non- significant (\(P> 0.05\)) [Table 1].
Most common clinical features were constipation seen in 36, bleeding PR in 28, bleeding PR weakness in 17, diarrhea in 16 and diarrhea + pain abdomen + weakness in 14 patients. The difference was non- significant (\(P> 0.05\)) [Table 2].
Table 1. Distribution of patients based on age group.
| Age group (years) | Number | P value |
|---|---|---|
| 11-20 | 8 | 0.82 |
| 21-30 | 22 | |
| 31-40 | 40 | |
| 41-50 | 24 | |
| <50 | 16 |
Table 2. Assessment of clinical profile.
| Clinical profile | Number | P value |
|---|---|---|
| Constipation | 36 | 0.72 |
| Bleeding PR | 28 | |
| Bleeding PR weakness | 17 | |
| Diarrhea | 16 | |
| Diarrhea + Pain abdomen + weakness | 14 |
Table 3. Distribution of non-neoplastic and neoplastic lesions.
| Parameters | Variables | Number | P value |
|---|---|---|---|
| Non-neoplastic (74) |
Non-specifc colitis | 22 | 0.05 |
| Ulcerative colitis | 16 | ||
| Acute inflammation | 14 | ||
| Hyperplastic polyp | 10 | ||
| Inflammatory polyp | 6 | ||
| Retention polyp | 4 | ||
| Endometriosis | 2 | ||
| Neoplastic benign (25) |
Benign spindle cell lesion | 3 | 0.02 |
| Tubular Adenoma | 15 | ||
| Villous Adenoma | 5 | ||
| Tubulovillous Adenoma | 2 | ||
| Neoplastic Malignant (13) |
Well differentiated adenocarcinoma | 4 | 0.04 |
| Moderately differentiated Adenocarcinoma | 6 | ||
| Poorly differentiated Adenocarcinoma | 2 | ||
| Signet ring cell Carcinoma | 1 |
Figure 1. Distribution of non-neoplastic and neoplastic lesions.
4. Discussion
Large intestine is affected by a long array of non-neoplastic and neoplastic lesions. Development of flexible fibreoptic sigmoidoscopy and colonoscopy revolutionized the diagnosis and management of colorectal diseases, for the reason that the procedure is safe with no serious complications [7, 8]. Application of therapeutic colonoscopy like colonoscopic polypectomy has replaced the open surgical procedure to a great extent [9, 10]. We performed clinico-pathological study of colonic biopsies.
Our results showed that age group 11-20 years had 8, 21-30 years had 22, 31-40 years had 40, 41-50 years had 24 and >50 years had 16 cases. Chandrakumari et al., [11] correlated histopathological spectrum of colonic mucosal biopsies with clinical findings. Out of 250 colonoscopic biopsies, 152 were non-neoplastic and 98 were neoplastic. Non neoplastic lesions were found to affect the colon most commonly. Most of the cases with non-neoplastic lesions presented with colicky abdominal pain, diarrhea and constipation. Among neoplastic lesions, 44 cases were benign and 54 cases were malignant. Majority of cases with neoplastic lesions presented with bleeding per rectum and constipation.
Our results showed that most common clinical features were constipation seen in 36, bleeding PR in 28, bleeding PR weakness in 17, diarrhea in 16 and diarrhea + pain abdomen + weakness in 14 patients. Makaju et al., [12] performed correlation between clinical and histopathological diagnosis of colorectal diseases. Analyses of 95 cases of colonoscopic biopsies were done. The most common clinical diagnosis was polyp in 49 cases (51.57%) and the common histopathological diagnosis was non-neoplastic polyps 31 (32.63%). There was no correlation in cases for suspected infectious colitis, microscopic colitis and hemorrhoids.
We observed that non-neoplastic lesions were 74. These were as non-specific colitis in 22, ulcerative colitis in 16, acute inflammation in 14, hyperplastic polyp in 10, inflammatory polyp in 6, retention polyp in 4 and endometriosis in 2 cases. Neoplastic benign lesions were 25. Benign spindle cell lesion was in 3, tubular adenoma in 15, villous adenoma in 5 and tubulovillous adenoma in 2 cases. Neoplastic malignant lesions were well differentiated adenocarcinoma seen in 4, moderately differentiated adenocarcinoma in 6, poorly differentiated adenocarcinoma in 2 and signet ring cell carcinoma in 1 case. Bhagyalakshmi et al., [13] evaluated normal and abnormal mucosal colonoscopic biopsy in the contribution of differential diagnosis in chronic diarrhea patients. Out of 104 biopsies evaluated, specific diagnoses were 41 (39.42%) and nonspecific diagnoses were 63 (60.57%). This study showed male preponderance (67% of cases) with average age of 40.5 years (6-84 years), remaining 33% female cases had average age 45 years (16-65 years). Out of 41 specific histological diagnoses made, majority of them were malignancies seen in the age group of 51-60 years and inflammatory bowel disease seen in the age group of 30-40 years.
Karve et al., [14] in their study a total of 159 colonoscopic biopsies were studied. Out of them, 68 (42.8%) were non neoplastic, 23 (14.4%) were benign lesions and 68 (42.8%) were malignant lesions. Among the 68 non neoplastic lesions, 32 cases were non-specific colitis, 11 cases ulcerative colitis, 5 cases juvenile polyps, 5 cases hyperplastic polyps, 4 cases SRUS, 3 cases granulomatous inflammation, 3 cases retention polyp, 2 cases Crohn's disease and one case each of acute inflammation, inflammatory polyp and endometriosis. Out of the 23 benign cases, 18were tubular adenomas (78.3%); 3 were villous adenomas (13%); 1 case of tubulovillous adenoma (4.3%) and 1 case of benign spindle cell lesion (4.3%). Out of 68 malignant lesions, 24 cases (35.3%) were well differentiated adenocarcinoma, 25 cases (36.8%) were moderately differentiated adenocarcinoma, 9 cases (13.2%) were poorly differentiated, 8 cases (11.8%) were mucin secreting adenocarcinoma and 2 cases (2.9%) were signet ring cell carcinoma.
5. Conclusion
Authors found that colonoscopy is a simple and a safe procedure. It helps in assessing the lesions clinically and confirming histopathologicaly through guided biopsy. Colonoscopic biopsies also play a key role not only in diagnosis, but also in follow up and treatment.Author Contributions:
All authors contributed equally to the writing of this paper. All authors read and approved the final manuscript.Conflicts of Interest:
"The authors declare no conflict of interest."References
- Patel, Y., Pettigrew, N. M., Grahame, G. R., & Bernstein, C. N. (1997). The diagnostic yield of lower endoscopy plus biopsy in nonbloody diarrhea. Gastrointestinal Endoscopy, 46(4), 338-343. [Google Scholor]
- Schmitt Jr, M. G., Wu, W. C., Geenen, J. E., & Hogan, W. J. (1975). Diagnostic colonoscopy: an assessment of the clinical indications. Gastroenterology, 69(3), 765-769. [Google Scholor]
- Kolhe, H. S., Mahore, S. D., Patil, S. S., & Patil, R. N. (2014). To study the endoscopic colonic biopsies of patients presenting with chronic watery diarrhea or constipation with special emphasis on microscopic colitis. IOSR Journal of Dental and Medical Sciences, 13(12), 84-88. [Google Scholor]
- Sood, A., Midha, V., Sood, N., Bhatia, A. S., & Avasthi, G. (2003). Incidence and prevalence of ulcerative colitis in Punjab, North India. Gut, 52(11), 1587-1590. [Google Scholor]
- Azad, S., Sood, N., & Sood, A. (2011). Biological and histological parameters as predictors of relapse in ulcerative colitis: a prospective study. Saudi Journal of Gastroenterology, 17(3), 194-198. [Google Scholor]
- Qayyum, A., & Sawan, A. S. (2009). Profile of colonic biopsies in King Abdul Aziz University Hospital, Jeddah. The Journal of the Pakistan Medical Association, 59(9), 608-611. [Google Scholor]
- Paudel, S. M. R., & Sharma, V. K. (2007). Ulcerative colitis is it the clinical problem in Nepal? Post-Graduate Medical Journal of NAMS, 7(2), 1-6. [Google Scholor]
- Rajbhandari, M., Karmacharya, A., Khanal, K., Dhakal, P., & Shrestha, R. (2013). Histomorphological profile of colonoscopic biopsies and pattern of colorectal carcinoma in Kavre district. Kathmandu University Medical Journal, 11(3), 196-200. [Google Scholor]
- Pandey, M. S., Pandey, A., & Dombale, V. D. (2016). Histomorphological profile of colonoscopic biopsies-a two year study in a tertiary care hospital in South India. International Journal of Science and Research, 5(2), 1513-1518. [Google Scholor]
- Badmapriya, D., & Kumar, V. S. (2011). Profile of ulcerative colitis in south indian region: karaikal. International Journal of Pharmacy and Biological Scinces, 1(2), 47-51. [Google Scholor]
- Roka, K., Indu, K. C., Jha, S. M., Subedi, R. C., & Adhikari, A. (2022). Pattern of lower Gastrointestinal diseases on colonoscopy and histopathological examination in a Ttertiary care center of Nepal. Medical Journal of Shree Birendra Hospital, 21(1), 87-92. [Google Scholor]
- Makaju, R., Amatya, M., Sharma, S., Dhakal, R., Bhandari, S., Shrestha, S., ... & Malla, B. (2017). Clinico-pathological correlation of colorectal diseases by colonoscopy and biopsy. Kathmandu University Medical Journal, 58(2), 173-178. [Google Scholor]
- Bhagyalakshmi, A., Venkatalakshmi, A., Praveen, L., & Sunilkumar, K. (2016). Clinico-pathological study of colonoscopic biopsies in patients with chronic diarrhea. Journal Research Medical Sciences, 4(7), 2738-2744. [Google Scholor]
- Karve, S. H., Vidya, K., Shivarudrappa, A. S., & Prakash, C. J. (2015). The Spectrum of colonic lesions: A Clinico-pathological study of colonic biopsies. Indian Journal of Pathology and Oncology, 2(4), 189-209. [Google Scholor]