Trends in Clinical and Medical Sciences
ISSN: 2791-0814 (online) 2791-0806 (Print)
DOI: 10.30538/psrp-tmcs2022.0036
COVID 19 associated mucormycosis: A curse in pandemic
Dhruvika Rathva\(^{1}\), Mayursinh Dodia\(^{1}\), Atisha Modi\(^{1}\) and Saudhan Desai\(^{2,*}\)
\(^{1}\) Department of Otorhinolaryngology, Parul Institute of Medical Sciences and Research, Parul University, Vadodara, Gujarat, India.
\(^2\) Department of Ophthalmology, Parul Institute of Medical Sciences and Research, Parul university, Vadodara, Gujarat, India.
Correspondence should be addressed to Saudhan Desai at drsaudhandesai@gmail.com
Abstract
Material and methods: Total twenty five patients with mucormycosis treated at tertiary care hospital in Gujarat during three months duration from May to July 2021. After detailed history thorough Ear, Nose and throat examination was performed. Along with local examination, ophthalmologic and neurologic examination performed in every case. After Functional endoscopic sinus surgery, tissue sent for histopathologic examination.
Results: Twenty five patients diagnosed with Mucormycosis, 18(72%) patients were males and 7(28%) were females. All 25(100%) had past history of COVID 19 infection and Diabetes Mellitus. Out of 25, 23(92%) patients were treated with intravenous or oral steroids and 2(8%) patients were not treated with any steroids. MRI paranasal sinuses with orbit with brain cuts performed for all 25 patients after suspicion of mucormycosis. 12(48%) patients had Sinonasal involvement, 11(44%) were Rhino-orbital involvement, and 2(8%) had Rhino palatal involvement. All 25(100%) patients were given Injection Amphotericin B for 3-4 weeks according to response. 6(24%) Patients were also given Oral Posaconazole. We performed Functional endoscopic sinus surgery in 23(92%) patients. In two (8%) cases Sinus surgery performed along with Maxillectomy. All 25(100%) cases on histopathology confirmed of Mucormycosis.
Conclusion: Prognostic factors we observed in our study were involvement of rhino-orbito-cerebral disease shows poor prognosis. Good Diabetes control showed early recovery. Early identification and early treatment improves prognosis as well as survival rates.
Keywords:
1. Introduction
Sinonasal mucormycosis is an acute invasive fungal infection which is rare, opportunistic and potentially fatal, that mostly occurs in immunocompromised patients[1]. Such immunocompromised patients are those with diabetes mellitus, prolonged corticosteroid therapy, solid organ transplant recipients, neutropenia and haematological malignancies[2]. Coronavirus disease (COVID-19), attributed to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was declared a global pandemic by the World Health Organisation(WHO) in March 2020[3].
In recent years, it was observed a surge regarding the incidence of mucormycosis infection; extracted evidence from multiple published epidemiological studies revealed a pooled prevalence of Coronavirus disease 2019 (COVID-19)-associated mucormycosis 50 times higher than before the pandemic era.The proposed mechanism of pathogenesis consists of inhalation of fungal spores from air that determine the colonization of respiratory mucosa at the level of the nasal cavity and paranasal sinuses and rapid spread to surround-ing structures, facilitated by its angio-invasive properties.Based on the anatomical region where mucormycosis has developed, it can be classified into rhino-orbito-cerebral, gastrointestinal, pulmonary, renal, cutaneous, disseminated. Other rare sites include ear, parotid gland, heart, lymph nodes, and bones.
This disease is caused by saprophytic and opportunistic fungi of class Phycomycetes, order mucorales, family mucoraceae belonging to genus mucor and rhizopus[4]. The fungus is angioinvasive and causes thrombosis of vessels, with consequent black necrosis of nasal and sinus tissue. Surgery, antifungals- intravenous along with topical therapy remains the main treatment options.
Untreated of severe cases of Mucormycosis can lead to cavernous sinus thrombosis, periorbital destruction, palatine ulcers, osteomyelitis, disseminated infection and eventually death.
2. Material and methods
Total twenty eight patients with suspected mucormycosis treated at tertiary care hospital in Gujarat during three months duration from May to July 2021. Out of which total 25 cases has been included in this study. Two patients died due to complications related to COVID 19 infection and also complications of mucormycosis, of these one patient had histopathologically proven Rhino-orbito-cerebral mucormycosis and other had radiologically suspected Pulmonary mucormycosis. Third patient had radiologically suspected Sinonasal mucormycosis but clinically and histopathologically turn out to be negative, so patient treated as Rhinosinusitis case.
So, after excluding above mentioned three cases, in this study total 25 patients were analysed. After detailed history thorough Ear, Nose and throat examination was performed. All patients were also evaluated by ophthalmologists and Infectious disease specialist. Along with local examination, ophthalmologic and neurologic examination performed in every case. All routine blood investigations were done, see Figures 1,2 and 3.
Figure 1. Case of right side periorbital oedema at presentation.
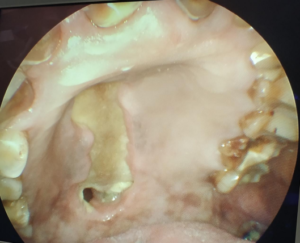
Figure 2. Figure showing palatal involvement.
Figure 3. Intraoperative finding of palatal involvement of another case.
3. Results
Twenty five patients diagnosed with Mucormycosis, 18(72%) patients were males and 7(28%) were females, see Table 1. Of all 25 cases Mean Age group 53 years $\pm$11standard deviation. All 25(100%) had past history of COVID 19 infection, But when came with mucormycosis related complaints, all patients RTPCR came negative. (Two patients diagnosed of mucormycosis on same presentation with COVID 19 with positive RTPCR report, but both expired during COVID 19 treatment, so excluded from study.) Clinical presentation observed in our cases was Nasal Obstruction 22 (88%), Nasal Discharge 2 (8%), Facial Pain 18 (72%), Facial Swelling 5 (20%), Vision Loss 1 (4%), Headache 21 (84%), Toothache 2 (8%), Periorbital Edema 7 (28%), see Table 2. All 25(100%) patients were also suffering from Diabetes Mellitus. Among 25 cases 8(32%) patients took treatment at Home in form of medications and home isolation for COVID 19 infection(one patient took oxygen therapy at home), one(4%) patient got admitted to hospital and stay was for less than 1 week. 16(64%) patients had COVID 19 related treatment at hospital with stay of 1-2 week. Total 18(72%) patients had to take Oxygen therapy for COVID 19 treatment, 7(28%) patients did not require O2 therapy. Out of 25, 23(92%) patients were treated with intravenous or oral steroids (Methyle presdnisolone/dexamethasone) and 2(8%) patients were not treated with any steroids. 14(56%) were given antiviral medications during COVID 19 treatment in form of Injection Remdesivir, 11(44%) patients did not require same. MRI paranasal sinuses with orbit with brain cuts performed for all 25 patients after suspicion of mucormycosis. 12(48%) patients had Sinonasal involvenment, 11(44%) were Rhino-orbital involvement, and 2(8%) had Rhino palatal involvement, see Table 3. All 25(100%) patients were given Injection Amphotericin B for 3-4 weeks according to response. 6(24%) Patients were also given Oral Posaconazole. We performed Functional endoscopic sinus surgery in 23(92%) patients. In two (8%) cases Sinus surgery performed along with Maxillectomy, see Table 4. All 25(100%) cases on histopathology confirmed of Mucormycosis. In case of Rhino orbital Mucormycosis 5(45%) patients were given retobulbar Amphotericin B injection on alternate day basis, for 2 weeks by Ophthalmologists, see Table 5. Advantages of performing surgery in mucormycosis cases are given in Table 6.Table 1. Associated comorbidities.
| Comorbidity | Male | Females | Total |
|---|---|---|---|
| Diabetes | 18 | 7 | 25 (100%) |
| Hypertension | 5 | 4 | 9 (36%) |
Table 2. Clinical presentation.
| Symptoms : | Patient No. (%) |
|---|---|
| Nasal Obstruction | 22 (88%) |
| Nasal Discharge | 2 (8%) |
| Facial Pain | 18 (72%) |
| Facial Swelling | 5 (20%) |
| Vision Loss | 1 (4%) |
| Headache | 21 (84%) |
| Toothache | 2 (8%) |
| Periorbital Edema | 7 (28%) |
Table 3. Disease extension based on MRI Findings.
| MRI fnding | Patient No. (%) |
|---|---|
| Sinonasal | 12 (48%) |
| Rhino Orbital | 11 ( 44%) |
| Rhino Palatal | 2 (8%) |
Table 4. Treatment outcome.
| Surgical : | Patient No. (%) |
|---|---|
| FESS | 23 (92%) |
| FESS + locally kept Amphotericin soaked gelfoam | 5(20%) |
| FESS + Maxillectomy | 2 (8%) |
| FESS + Retrobulbar Amphotericin Inj. | 5 (20%) |
Table 5. Treatment outcome.
| Medical: | Patient No. (%) |
|---|---|
| Inj Amphotericin B | 25 (100%) |
| Oral Posaconazle | 6 (24%) |
Table 6. Advantages of performing surgery in mucormycosis cases.
| i. | Better penetration of Antifungal medications |
|---|---|
| ii. | Slows down disease progression and restricts the extent allowing time for bone marrow regeneration |
| iii. | Reduces the fungal load which reduces load on recovering neutrophils |
| iv. | Provides a specimen for histopathology |
4. Discussion
Along with increase in the novel coronavirus (COVID - 19) cases, number of opportunistic fungal infections appears to be raised. Globally, several cases of mucormycosis have been observed in patients with COVID-19, the term being used is COVID-19 associated mucormycosis (CAM). Mucormycosis has been declared an epidemic in several Indian states and has been classified as a notifiable disease. Early diagnosis and prompt initiation of treatment is crucial as the condition can progress rapidly with fatal outcome. The etiology of the sudden rise of mucormycosis in India appears to be multifactorial in nature with several hypothesis linking mucormycosis to severe Covid-19 patients who are immune compromised and/or have associated co-morbidities. For example, diabetes, which is a known risk factor for Covid, is also found to be strongly associated with risk of mucormycosis. According to the WHO[5], about 1.5 million deaths were attributed to diabetes globally, and its prevalence is increasing rapidly in low- and middle-income countries. India, home to over 77 million diabetics, has the second highest number of diabetics in the world next to China[6] and that the prevalence of diabetes in India is on the rapid rise[7].
In our study majority of patients were a male, which is similar to study by Pal et al.,[8]. We observed that all our cases were related to COVID-19 infection, majority of patients had suffered from disease. So Mucormycosis linked with it. Our all cases had associated diabetes mellitus, observed in all 25(100%) cases. Hyperglycemia, as seen in patients with uncontrolled diabetes mellitus, leads to phagocyte dysfunction, impaired chemotaxis and defective intracellular killing by oxidative and non-oxidative mechanisms[9]. Although data on the degree of glycemic control were infrequently reported across all the included studies, it is expected that COVID-19 might have further worsened the glucose profile of the patients with diabetes, thereby further predisposing them to mucormycosis. SARS-CoV-2 can infect and replicate in the human islet cells, leading to $\beta$-cell damage and reduced endogenous insulin secretion. Besides, the plethora of cytokines, as seen in patients with COVID-19, can lead to worsening of insulin resistance.% with COVID-19, can lead to worsening of insulin resistance.
Usually elevated in patients with severe COVID-19, interleukin-6 (IL-6) causes insulin resistance by impairing the phosphorylation of insulin receptor and insulin receptor substrate-1[10].
The use of glucocorticoids is a known risk factor for the development of mucormycosis[11]. Glucocorticoid-induced immunosuppression, hyperglycaemia and lymphopenia predispose to the pathogenesis of mucormycosis. The rampant use of glucocorticoids in patients with COVID-19 has undoubtedly contributed to the upsurge in the number of cases of CAM. Another indirect association between the concomitant surge in COVID-19 and mucormycosis is the dissemination of fungal spores via water used in oxygen humidifiers. Indeed, hospital water is a potential reservoir for fungi including Mucorales[12]. After such study found, in our hospital we used distilled water in oxygen humidifiers in COVID affected patients. We could not find out its actual relation in occurrence of post COVID-19 mucormycosis, due to lack of proper follow up of cases that were treated with only oxygen therapy for COVID 19 infections.
The 1950 Smith and Krichner criteria[13] for the clinical diagnosis of mucormycosis are still considered to be gold standard and include: \begin{description}
In our study 12(48%) patients had Sinonasal involvement, 11(44%) had Rhino-orbital involvement, and 2(8%) had Rhino palatal involvement. These findings are similar to study by Abha et al.,[15], where most common sino-nasal disease involvement followed by rhino-orbital disease. In all our cases we performed Functional endoscopic sinus surgery. Advantages described in Table \ref{tab5}. In case of palatal involvement, after maxillectomy obturator was given to cover defect & to prevent nasal regurgitation.
Despite recent tremendous advancements in sinus surgery, invasive fungal sinusitis still has a high mortality rate. So, many researchers have recommended sinus surgery/debridement and long-term antifungal treatment. These might cause severe morbidity and complications, so some treatment techniques have been modified in order to gain better clinical outcomes. Direct introduction of amphotericin B to the sinus cavity is one of the options which we followed. We did it in 5(20%) cases, which showed better outcome. Those patients had early recovery. After surgery, local area packed with gelfoam soaked in Amphotericin B(50mg vial of Amphotericin B diluted in 10ml of sterile water). This method helps in reducing density of fungal spores. Many researchers have used topical treatment, but well designed, controlled studies are needed to evaluate patients responses to this type of treatment.
All 25 patients treated with Injectable Amphotericin B, with dose of 1 mg/kg/day or Liposomal Amphotericin B 3-5mg/kg/day for 2-3 weeks. Liposomal or conventional injection usage, decided on basis of availability, cost and comorbidities of patients. Amphotericin B acts by binding to ergosterol in the cell membrane of fungi. After binding with ergosterol, it causes the formation of ion channels leading to loss of protons and monovalent cations, which results in depolarization and concentration-dependent cell killing. Additionally, amphotericin B also produces oxidative damage to the cells with the formation of free radicals and subsequently increased membrane permeability. Amphotericin B also has a stimulatory effect on phagocytic cells, which assists in fungal infection clearance.The half-life of amphotericin B is from 24 hours to 15 days.
Infusion related reactions occur in few cases. Such reactions can be rigor, chills, fever, headache, nausea, malaise or generalised rashes. Reactions can be avoided or minimized by premedication with aspirin or ibuprofen or by adding 25mg of hydrocortisone to the infusion directly[13]. We did not notice any kind of infusion related reactions in our patients receiving Injection Amphotericin B. Oral Posaconazole(800mg per day) can be used for salvage treatment in patients who are intolerant to Amphotericin B. It can also be used as a step down therapy after initial control of the disease with Amphotericin B. We used oral Posaconazole in 6(24%) cases after initial control with Injection Amphotericin B. Oral Isavuconazole also being better option, but not used in any case due to unavailability.
Hyperbaric oxygen has been used as an adjunct to the current therapeutic approach of aggressive surgical debridement, Amphotericin B therapy and control of underlying predisposing conditions. Although studies have shown that hyperbaric oxygen exerts a fungistatic effect, its most important effect is to aid neovascularization with subsequent healing in poorly perfused acidotic and hypoxicbut viable tissue. Hyperbaric oxygen therapy for mucormycosis should consist of exposure to 100% oxygen for 90 min to 2 hour at pressures of 2.0-2.5 atmospheres with one or two exposures daily for a total of 40 treatments. Reported toxicities of hyperbaric oxygen include teratogenicity and, rarely, pulmonary or CNS side-effects. Although hyperbaric oxygen is offered by only a few medical facilities, it may be warranted in patients who appear to be deteriorating despite maximal surgical and medical therapy[16]. Though we did not treat any case of mucormycosis with Hyperbaric oxygen therapy.
Antifungal therapy started only after KOH or histopathological confirmed cases of Mucor. On histopathology, the fungal hyphae seen as broad, ribbon like, irregular and aseptate with branching at right angle. On KOH also broad, aseptate hyphae seen.
To note, our study has few limitations. 25 cases in this study can be considered as small sample size. This disease seen rarely in past but post COVID 19 era rapid surge was seen. High cost treatment is one of factor for less number of patients. Being an observational study there is no control group to evaluate differences.
5. Key message
- Mucormycosis is a rare and occasionally fatal opportunistic infection that affects immunocompromised patients. Most patients who encounter mucormycosis are diabetic with uncontrolled diabetes. Occurrence of many cases of mucormycosis was a curse in already bad situation of COVID 19 infection, which lead to significant morbidity.
- In the COVID-19 era, the rate of mucormycosis seems to be increasing, and the earlier the presentation to hospitals, the better the outcome. Early surgical debridement and antifungal therapy is must for treatment. Use of steroids in COVID 19 related cases was like walking on double edge sword. So, A standard dose recommended by the World Health Organization based on the RECOVERY trial that is 6 mg of dexamethasone once daily for no more than 7-10 days should be strictly adhered to and lower doses should be considered in immunocompromised or diabetic patients.
- Prognostic factors we observed in our study were; involvement of rhino-orbito-cerebral disease shows poor prognosis. Good Diabetes control showed early recovery. Early identification and early treatment improves prognosis as well as survival rates.
- Disclosure of potential conflicts of interest: All authors declare that they have no conflicts of interest.
- Informed Consent: Informed consent was obtained from all individual participants included in the study. Additional informed consent was obtained from one participant whose identifying information is included in this article.
- Sources of funding: None
- Ethical approval: All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional ethics committee and with the 1964 Helsinki declaration.
Author Contributions:
All authors contributed equally to the writing of this paper. All authors read and approved the final manuscript.Conflicts of Interest:
"The authors declare no conflict of interest."References
- Singh, V. P., Bansal, C., & Kaintura, M. (2019). Sinonasal mucormycosis: A to Z. Indian Journal of Otolaryngology and Head & Neck Surgery, 71(Suppl 3), 1962-1971.[Google Scholor]
- Selarka, L., Sharma, S., Saini, D., Sharma, S., Batra, A., Waghmare, V. T., ... & Ong, J. J. (2021). Mucormycosis and COVID-19: an epidemic within a pandemic in India. Mycoses, 64(10), 1253-1260.[Google Scholor]
- WHO. Listing of WHO's response to COVID-19. Publised 2020. Accessed May 16, 2021.
- Soni, A. (2017). Paranasal mucormycosis in an immunocompetent individual: Importance of early diagnosis. International Journal of Medical and Oral Research, 4(3), 52-56.[Google Scholor]
- WHO. Diabetes fact-sheets. Published 2021. Accessed May 26, 2021. https://www.who.int/news-room/fact-sheets/details/diabetes. [Google Scholor] 2021.
- Statista. Countries with highest number of Diabetics worldwide. Published 2019. Accessed May 26, 2021.
- Tandon, N., Anjana, R. M., Mohan, V., Kaur, T., Afshin, A., Ong, K., ... & Dandona, L. (2018). The increasing burden of diabetes and variations among the states of India: the Global Burden of Disease Study 1990--2016. The Lancet Global Health, 6(12), e1352-e1362.[Google Scholor]
- Pal, R., Singh, B., Bhadada, S. K., Banerjee, M., Bhogal, R. S., Hage, N., & Kumar, A. (2021). COVID-19-associated mucormycosis: an updated systematic review of literature. Mycoses, 64(12), 1452-1459.[Google Scholor]
- Chinn, R. Y., & Diamond, R. D. (1982). Generation of chemotactic factors by Rhizopus oryzae in the presence and absence of serum: relationship to hyphal damage mediated by human neutrophils and effects of hyperglycemia and ketoacidosis. Infection and immunity, 38(3), 1123-1129.[Google Scholor]
- Rehman, K., Akash, M. S. H., Liaqat, A., Kamal, S., Qadir, M. I., & Rasul, A. (2017). Role of interleukin--6 in development of insulin resistance and type 2 diabetes mellitus. Critical Reviews in Eukaryotic Gene Expression, 27(3), 229--236.(3), 229--236.[Google Scholor]
- Ibrahim, A. S., Spellberg, B., & Walsh, T. J. DP (2012). Kontoyiannis, pathogenesis of mucormycosis. Clinical Infectious Diseases, 54, S16-S22.[Google Scholor]
- Rammaert, B., Lanternier, F., Zahar, J. R., Dannaoui, E., Bougnoux, M. E., Lecuit, M., & Lortholary, O. (2012). Healthcare-associated mucormycosis. Clinical Infectious Diseases, 54(suppl\_1), S44-S54.[Google Scholor]
- Smith, H. W., & Kirchner, J. A. (1958). Cerebral mucormycosis: a report of three cases. AMA Archives of Otolaryngology, 68(6), 715-726.[Google Scholor]
- Parsi, K., Itgampalli, R. K., Vittal, R., & Kumar, A. (2013). Perineural spread of rhino-orbitocerebral mucormycosis caused by Apophysomyces elegans. Annals of Indian Academy of Neurology, 16(3), 414-417.[Google Scholor]
- Kumari, A., Rao, N. P., Patnaik, U., Malik, V., Tevatia, M. S., Thakur, S., ... & Saxena, P. (2021). Management outcomes of mucormycosis in COVID-19 patients: A preliminary report from a tertiary care hospital. Medical Journal Armed Forces India, 77, S289-S295.[Google Scholor]
- Greenberg, R. N., Scott, L. J., Vaughn, H. H., & Ribes, J. A. (2004). Zygomycosis (mucormycosis): emerging clinical importance and new treatments. Current Opinion in Infectious Diseases, 17(6), 517-525.[Google Scholor]