Trends in Clinical and Medical Sciences
ISSN: 2791-0814 (online) 2791-0806 (Print)
DOI: 10.30538/psrp-tmcs2022.0033
Major bacteriological isolates and their antimicrobial susceptibility trends in ICU of a tertiary care hospital: A prospective observational study
Kirti Ahuja\(^{1}\), Prateek\(^{1}\), Meena Singh\(^{1}\), Anil Kumar Verma\(^{2,*}\), Pranav Bansal\(^{1}\) and Sanjay\(^{3}\)
\(^{1}\) Department of Anaesthesiology, Govt Medical College for Women, Khanpur Kalan, Sonepat, India.
\(^{2}\) Department of Anaesthesia, GSVM Medical College Kanpur UP India.
\(^{3}\) Department of Orthpaedics, N.C. Medical College, Israna, Panipat, India.
Correspondence should be addressed to Anil Kumar Verma at kirtiahuja2812@gmail.com
Abstract
Keywords:
1. Introduction
Bloodstream infection is one of the principal causes of morbidity and mortality in the intensive care unit. Critical care patients are often associated with an increasing number of invasive devices and monitors that make them five to seven-fold more susceptible to acquisition of nosocomial infection as compared to general inpatients in the hospital [1, 2]. The Surviving sepsis campaign guidelines, ever since its inception, have emphasised the initiation of antibacterial therapy within the first hour of presentation to the hospital for better/improved survival [3]. But, the institution of an inappropriate empirical antimicrobial therapy has been associated with a five-fold reduction in survival. Rapid and accurate identification of bacterial species in the blood is, therefore, of paramount importance [4].
Since, microbiological culture results are not available until after 24 to 72 hours, the initial therapy for infection is often empirical and guided by the clinical presentation. Broad-spectrum antimicrobial agents are generally started initially with the intent to cover most pathogens commonly associated with specific clinical syndromes. Nonetheless, the irrational and inappropriate usage of antibiotics has resulted in rising trend of resistant organisms especially in critical care settings [5, 6]. Therefore, once the identity of the etiologic pathogen and the antimicrobial susceptibility data are available, every attempt should be made to narrow down the antibiotic spectrum. This is a critical component of antibiotic therapy through which a reduction in the cost, toxicity and development of antimicrobial resistance in the community can be accomplished.
The micro-organisms and their antibiotic susceptibility pattern vary among different healthcare facilities and geographical areas. The antibiograms provide a summary of in vitro activity of antimicrobials of an institution or geographical area. So, the decisions regarding initial antimicrobial therapy should be based on the institution's specific antibiograms. Clinicians must choose empirical antibiotic therapy aimed at both maximizing outcomes and minimizing the emergence of resistance. With blood culture being one of the most reliable investigations for bacterial isolation and detection, we designed the present study to determine the bacterial profile of bloodstream infections (BSI) and their antibiotic susceptibility patterns among the clinically diagnosed cases of sepsis in patients presenting to our surgical intensive care unit (ICU) to direct the antibiotic treatment of hospital acquired infections in the ICU.
2. Materials and methods
After approval from institutional ethical committee, this prospective study was conducted over a period of eighteen months in the 6- bedded surgical ICU of a tertiary care hospital. All patients of either sex between the age of 15-60 years, admitted to the ICU during the study period were included. Patients shifted to ICU for monitoring during postoperative period, mortality within 24 hours of admission and patients transferred to another speciality team were excluded. Written informed consent was obtained from either the patient or relatives of the included patients. The blood culture sample of these patients were collected when the patient presented with any two of the following four features,alongwitha suspected source of infection i.e. temperature>38$^{o}$C or< 36$^{o}$C, heart rate >90 beats/min, respiratory rate >24/min and Total leucocyte counts >12000/cu mm or < 4000/cu mm.
Collection of blood sample for blood culture was done using standard aseptic techniques. 10 ml of blood specimen was collected and inoculated into brain heart infusion (BHI) broth at the blood to broth ratio of 1:10. After incubation at 37$^{o}$C for 24 and 48hours, blind subcultures were made on Macconkey agar and blood agar plates (Hi Media Laboratories, India). After 24 hrs of aerobic incubation at 37$^{o}$C, the plates were observed for bacterial growth. Identification of significant isolates and their antimicrobial susceptibility tests was carried out as per Clinical and Laboratory Standards Institute (CLSI) guidelines, 2012 [7]. Antimicrobial sensitivity patterns of isolated organisms were identified by Kirby Bauer's disc diffusion method on Mueller Hinton Agar media [8]. Interpretations of antibiotic susceptibility results were made according to the guidelines of interpretative zone diameters of CLSI [7]. Antibiotics that were tested in this study include Amoxycillin-sulbactam, Cefuroxime, ceftriaxone,cefoperazone-sulbactum,cefipime,cefazolin,ceftazidime,piperacillin-tazobactum,imepenem, meropenem, linezolid, clarithromycin, azithromycin, clindamycin, norfloxacin, ofloxacin, levofloxacin, sparfloxacin, gentamycin, amikacin, tobramycin, netilmycin, tigecycline, nitrofurantion, colistin, polymyxin-B, and vancomycin.
3. Data collection and analysis
Standard descriptive statistics were calculated for categorical (in percentage) and continuous variables (median and interquartile range). Prevalence rate was calculated for the numbers of positive cases of examined subjects. Antibiogram, which provides the percentage of isolates that are susceptible to an antibiotic, was constructed according to consensus guidelines from the Clinical Laboratory Standards Institute.4. Results
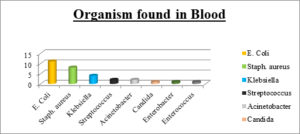
A total of 140 blood samples of the patients with suspectedbacteraemia, admitted to the critical care unit were sent for processing of blood culture to the department of Microbiology. The median age of the patients in our study was 31.9 years (range 23.5-44.5 years), while 65% were male.Ninety five (67.86%) patients were admitted secondary to traumatic brain injury while forty five (32.14%) patients were postoperative cases. Figure \ref{f1} shows that out of the 140 blood cultures sent during the study period, 30 (21.43%) were positive for significant growth of pathogen suggesting bloodstream infection (BSI). In this, 29(96.67%) were bacterial and 1(3.33%) was fungal (candida nonalbicans). Among the bacterial isolates, Gram negative bacteria (GNB)(60%) were the leading pathogenic agents with E. coli (11cultures, 36.67%) being the most common followed by Klebsiella species (4 cultures, 13.3%), and Acinetobacter species (2 cultures, 6.67%).Gram positive bacteria (GPB) were isolated in 36% of the samples, wherein staphylococcus aureus (8 cultures, 26.67%) was the main pathogen followed by streptococcus (2 cultures, 6.675%).Figure 1. Organisms in Bloodstream infection.
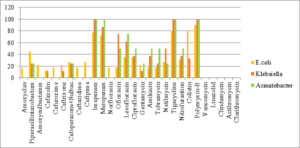
Figure 2. Antibiogram of gram negative bacteria in blood.
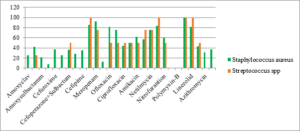
Figure 3. Antibiogram of gram positive bacteria in blood.
Table 1. Antimicrobial susceptibility of major bacterial isolates in blood.
| Amoxyclav | Piperacillintazo | Amoxysulbactamm | Cefazolin | Cefuroxime | Ceftrixone | Cefoperazone+Sulbactum | Ceftazidime | Cefpime | Imepenem | Meropenam | Norfloxacin | Ofloxacin | Levofloxacin | ciprofloxacin | Gentamycin | Amikacin | tobramycin | netilmycin | Tigecycline | nitrofurantion | Colistin | Polymyxin-B | Vancomycin | Linezolid | Clindamycin | Azithromycin | Clarithromycin | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| E.coli(11) | 18 | 45 | 22 | 13 | 18 | 22 | 27 | 18 | 27 | 77 | 72 | 18 | 18 | 36 | 36 | 22 | 18 | 18 | 27 | 81 | 31 | 81 | 90 | ||||||
| Staphylococcus aureus(8) | 25 | 42 | 21 | 8 | 37 | 25 | 36 | 28 | 35 | 85 | 92 | 13 | 81 | 75 | 44 | 50 | 62 | 57 | 75 | 83 | 60 | 100 | 81 | 43 | 31 | 37 | |||
| Klebsiella(4) | 0 | 25 | 0 | 12 | 0 | 12 | 25 | 0 | 0 | 100 | 87 | 0 | 75 | 62 | 37 | 12 | 37 | 25 | 50 | 100 | 37 | 33 | 100 | ||||||
| Streptococcus spp(2) | 0 | 25 | 0 | 0 | 0 | 0 | 50 | 0 | 0 | 100 | 75 | 0 | 50 | 50 | 50 | 50 | 50 | 75 | 75 | 100 | 50 | 100 | 100 | 50 | |||||
| Acinetobacter(2) | 0 | 25 | 0 | 0 | 0 | 25 | 25 | 25 | 0 | 100 | 100 | 50 | 50 | 75 | 50 | 25 | 50 | 50 | 25 | 100 | 50 | 50 | 100 |
5. Discussion
Nosocomial infections cause significant morbidity and mortality in patients admitted to ICUs worldwide. Antibiotics form a considerable portion of the immense economic burden borne by these patients [5]. However, inappropriate use of antibiotics may lead to antimicrobial resistance causing increasing mortality and healthcare costs. This study was undertaken to study the spectrum of the bacterial isolates causing blood stream infection in ICU patients and their antibiotic susceptibility pattern which could guide the formulation of antibiogram and future antibiotic policy.The Blood culture positivity rate in our study was observed to be 21.43% which was similar to the studies conducted by Alam et al., and others [10, 11, 12]. Though these were lower than the incidence observed by Parihar et al., and others [13,14, 15, 16, 17]. But, these blood culture rates were however higher as compared to a few other studies where the blood culture positive rates ranged only from 9.94% - 11.2% [18, 19, 20]. These differences in the positivity rates may be due to the difference in methodology used for blood culture, the study design, nature of patient population, epidemiological difference in etiological agents, geographical differences and differences in the infection control policies [19, 20, 21].
In our study, 60% of the infections were caused by GNBand36.67% of the infection was due to GPB. This finding was comparable to most of the studies from India and other developing countries, where Gram-negative bacteria have been reported to be the most common cause of bacteraemia in hospitalized patients [21, 22, 23]. In contrast, Arora et al., [11] and Shrestha et al., [17] have reported gram positive bacterial dominance in blood stream infections. Escherichia coli (36.67%) was the predominant Gram-negative isolate in our study, followed by Klebsiella (13.33%). These findings are in concordance with findings of Gupta et al., [23]. However, some other studies have isolated Pseudomonas and Acinetobacter predominantly [24]. This may be due to different antibiotic prescription policies. In GPB isolates, Staphylococcus aureus (26.67%) formed the majority followed by Streptococcus (6.67%). Similar findings were reported by Gupta et al., and Parihar et al., [23, 13], that Candida was seen in 3.33% of positive blood culture and all were non albicans Candida species.
Antibiotic resistance is a major concern in ICU worldwide and especially in India. Critical care areas are the major foci of antimicrobial resistance in hospitals [1]25,26}. Overuse of antibiotics is the leading cause of selection pressure on organisms and thereby, antimicrobial resistance [1]27}.
All the three major GNB isolates; E.coli, Klebsiella and Acinetobacter showed high degree of resistance to penicillins, cephalosporins and piperacillin-tazobactum. Susceptibility to levofloxacin, ofloxacin, amikacin and netilmycin ranged from intermediate to high in Klebsiella and Acinetobacter while E coli showed high resistance. Similar findings were noted by Parajuli et al., [17]. The increasing resistance to Colistin is a troublesome finding as it further decreases the antimicrobials available in our armamentarium for treatment of infections, especially multidrug resistant variants. On the positive side, all the three GNB isolates demonstrated higher susceptibility to Carbapenems, tigecycline and polymixin B. This is in contrast to studies [24, 25, 26, 27, 28, 29], which showed high level of resistance to Carbapenems. The low resistance to Carbapenems in our study could be attributed in part to the practice of administering the Carbapenems as infusions in our institute which has shown to limit the resistance to these antibiotics.
Both GPBisolates, staphylococcus and streptococcus showed high resistance to penicillins, cephalosporins and macrolides. The sensitivity for aminoglycosides, clindamycin and fluoroquinolones was intermediate with higher sensitivity noted to ofloxacin and levofloxacin. However, the sensitivity to Carbapenems, tigecyclin, linezolid and vancomycin was as high as upto100%. The high degree of resistance to $\beta$-lactams, most cephalosporins, and increasing resistance to fluoroquinolones and aminoglycosides among both GPB and GNB in our study was also established in many other studies, see [11, 27, 28, 29]. This is probably because these are the most frequently prescribed antibiotics in developing nations. Another frequently observedissue in developing nations is the easy availability of antibiotics as over the counter preparations.
6. Conclusion
Gram negative bacterial isolates are the most common organism found in our study followed by gram positive bacteria. E coli being the predominant organism followed by staphylococcus aureus, Klebsiella, streptococcus and Acinetobacter.Antibiogramdepicts gram negative organism have maximum sensitivity towards polymyxin followed by Carbapenems and piperacillin-tazobactum in decreasing order and gram positive bacteria have maximum sensitivity to vancomycin and linezolid followed by Carbapenems, piperacillin-tazobactum.Appropriate and targeted antimicrobial therapy initiated early can be life-saving. However, the high prevalence of multidrug resistance microbes highlight our limited treatment options. Proper antimicrobial stewardship can be a step forward towards antimicrobial resistance containment. Routine surveillance to know the local epidemiology and baseline resistance of the pathogens for formulation of local antibiogram and hospital antibiotic policy will go a long way in combating growing antimicrobial resistance and curtailing rising costs in critical care.Author Contributions:
All authors contributed equally to the writing of this paper. All authors read and approved the final manuscript.Conflicts of Interest:
"The authors declare no conflict of interest."References
- Günseren, F., Mamıkoğlu, L., Öztürk, S., Yücesoy, M., Biberoğlu, K., Yuluğ, N., ... & Günaydın, M. (1999). A surveillance study of antimicrobial resistance of gram-negative bacteria isolated from intensive care units in eight hospitals in Turkey. Journal of Antimicrobial Chemotherapy, 43(3), 373-378.[Google Scholor]
- Kumar, A., Ellis, P., Arabi, Y., Roberts, D., Light, B., Parrillo, J. E., ... & Cooperative Antimicrobial Therapy of Septic Shock Database Research Group. (2009). Initiation of inappropriate antimicrobial therapy results in a fivefold reduction of survival in human septic shock. Chest, 136(5), 1237-1248.[Google Scholor]
- Lehman, K. D. (2019). Update: surviving sepsis campaign recommends hour-1 bundle use. The Nurse Practitioner, 44(4), 10. [Google Scholor]
- Trenholme, G. M., Kaplan, R. L., Karakusis, P. H., Stine, T., Fuhrer, J., Landau, W., & Levin, S. (1989). Clinical impact of rapid identification and susceptibility testing of bacterial blood culture isolates. Journal of Clinical Microbiology, 27(6), 1342-1345.[Google Scholor]
- Barai, L., Fatema, K., Haq, J. A., Faruq, M. O., Ahsan, A. A., Morshed, M. A. H. G., & Hossain, M. B. (2010). Bacterial profile and their antimicrobial resistance pattern in an intensive care unit of a tertiary care hospital of Dhaka. Ibrahim Medical College Journal, 4(2), 66-69.[Google Scholor]
- Gudiol, C., & Carratala, J. (2014). Antibiotic resistance in cancer patients. Expert Review of Anti-Infective Therapy, 12(8), 1003-1016. [Google Scholor]
- Wikler, M. A., Cockerill, F. R., & Craig, W. A. (2008). Clinical and laboratory standards institute. Performance Standards for Antimicrobial Susceptibility Testing: Eighteenth Informational Supplement. Wayne: Clinical and Laboratory Standards Institute. [Google Scholor]
- Bauer, A. W., Kirby, W. M., Sherris, J. C., & Turck, M. (1966). Antibiotic susceptibility testing by a standardized single disk method. American Journal of Clinical Pathology, 45(4), 493. [Google Scholor]
- Shalini, S., Kranthi, K., & Gopalkrishna, B. K. (2010). The microbiological profile of nosocomial infections in the intensive care unit. Journal of Clinical and Diagnostic Research, 4(5), 3109-3112. [Google Scholor]
- Alam, M. S., Pillai, P. K., Kapur, P., & Pillai, K. K. (2011). Resistant patterns of bacteria isolated from bloodstream infections at a university hospital in Delhi. Journal of Pharmacy & Bioallied Sciences, 3(4), 525-530. [Google Scholor]
- Arora, U., & Devi, P. (2007). Bacterial profile of blood stream infections and antibiotic resistance pattern of isolates. JK Science, 9(4), 186-190.[Google Scholor]
- Fayyaz, M., Mirza, I. A., Ikram, A., Hussain, A., Ghafoor, T., & Shujat, U. (2013). Pathogens causing blood stream infections and their drug susceptibility profile in immunocompromised patients. Journal of the College of Physicians and Surgeons Pakistan, 23(12), 848-51.[Google Scholor]
- Parihar, R. S., Agrawal, R., Khatri, P. K., Soni, P., Duggal, S., & Dhoundyal, R. (2015). Rapid identification of clinically important aerobic microorganisms by automated blood culture system and their antimicrobial resistance pattern at tertiary care hospital at Western Rajasthan India. Journal of Medical Science and Clinical Research, 3, 6359-6366. [Google Scholor]
- Ramana, K. V., Rao, S. D., Vaish, R., & Rao, B. M. (2015). Performance Analysis of Blood Culture by an Automated Blood Culture System at a Tertiary Care Teaching Hospital in South India. American Journal of Clinical Medicine Research, 3(3), 45-49.[Google Scholor]
- Mittal, P., & Sharma, A. (2017). Bacteriological profile and antimicrobial susceptibility of blood culture isolates from the patients of tertiary care hospital, Udaipur. International Journal of Recent Trends in Science and Technology, 23(1), 24-28. [Google Scholor]
- Vasudeva, N., Nirwan, P. S., & Shrivastava, P. (2016). Bloodstream infections and antimicrobial sensitivity patterns in a tertiary care hospital of India. Therapeutic Advances in Infectious Disease, 3(5), 119-127. [Google Scholor]
- Wasihun, A. G., Wlekidan, L. N., Gebremariam, S. A., Dejene, T. A., Welderufael, A. L., Haile, T. D., & Muthupandian, S. (2015). Bacteriological profile and antimicrobial susceptibility patterns of blood culture isolates among febrile patients in Mekelle Hospital, Northern Ethiopia. Springerplus, 4, Article No. 314. [Google Scholor]
- Mehta, M., Dutta, P., & Gupta, V. (2005). Antimicrobial susceptibility pattern of blood isolates from a teaching hospital in North India. Japanese Journal of Infectious Diseases, 58(3), 174-176. [Google Scholor]
- Ghadiri, H., Vaez, H., Khosravi, S., & Soleymani, E. (2012). The antibiotic resistance profiles of bacterial strains isolated from patients with hospital-acquired bloodstream and urinary tract infections. Critical Care Research and Practice, 2012, Article ID 890797 . [Google Scholor]
- Gohel, K., Jojera, A., Soni, S., Gang, S., Sabnis, R., & Desai, M. (2014). Bacteriological profile and drug resistance patterns of blood culture isolates in a tertiary care nephrourology teaching institute. BioMed Research International, 2014, Article ID 153747. [Google Scholor]
- Zenebe, T., Kannan, S., Yilma, D., & Beyene, G. (2011). Invasive bacterial pathogens and their antibiotic susceptibility patterns in Jimma University specialized hospital, Jimma, Southwest Ethiopia. Ethiopian Journal of Health Sciences, 21(1), 1-8. [Google Scholor]
- Dagnew, M., Yismaw, G., Gizachew, M., Gadisa, A., Abebe, T., Tadesse, T., ... & Mathewos, B. (2013). Bacterial profile and antimicrobial susceptibility pattern in septicemia suspected patients attending Gondar University Hospital, Northwest Ethiopia. BMC Research Notes, 6, Article No. 283. [Google Scholor]
- Gupta, S., & Kashyap, B. (2016). Bacteriological profile and antibiogram of blood culture isolates from a tertiary care hospital of North India. Tropical Journal of Medical Research, 19(2), 94-99. [Google Scholor]
- Jain, A., Agarwal, A., Verma, R. K., Awasthi, S., & Singh, K. P. (2011). Intravenous device associated blood stream staphylococcal infection in paediatric patients. The Indian Journal of Medical Research, 134(2), 193-199. [Google Scholor]
- Irfan, S., Idrees, F., Mehraj, V., Habib, F., Adil, S., & Hasan, R. (2008). Emergence of Carbapenem resistant Gram negative and vancomycin resistant Gram positive organisms in bacteremic isolates of febrile neutropenic patients: a descriptive study. BMC Infectious Diseases, 8, [Google Scholor]
- Bansal, S., & Advani, S. H. (2014). Pattern of bloodstream infections in patients with hematological malignancies in a tertiary care centre. Indian Journal of Cancer, 51(4), 447-449. [Google Scholor]
- Parajuli, N. P., Parajuli, H., Pandit, R., Shakya, J., & Khanal, P. R. (2017). Evaluating the trends of bloodstream infections among pediatric and adult patients at a teaching hospital of Kathmandu, Nepal: role of drug resistant pathogens. Canadian Journal of Infectious Diseases and Medical Microbiology, 2017, Article ID 8763135. [Google Scholor]
- Garg, V. K., Mishra, S., Gupta, N., Garg, R., Sachidanand, B., Vinod, K., ... & Bhatnagar, S. (2019). Microbial and antibiotic susceptibility profile among isolates of clinical samples of cancer patients admitted in the intensive care unit at regional tertiary care cancer center: a retrospective observational study. Indian Journal of Critical Care Medicine, 23(2), 67-72. [Google Scholor]
- Jadhav, S., Gandham, N., Paul, R., Misra, R. N., Ujagare, M. T., & Angadi, K. (2012). Bacteriological profile of septicaemia and antimicrobial susceptibility of isolates from tertiary care hospital in India. Research Journal of Pharmaceutical, Biological and Chemical Sciences, 3, 1100-1108.