For timely prediction of the development of AHI syndrome in patients with closed abdominal trauma, it is necessary to monitor the IAP level. IBH syndrome develops in patients with concomitant abdominal trauma and is characterized by relatively high mortality rates. A statistically significant correlation was established between the level of AHI, APD, the frequency of development of a picture of multiple organ failure, and the severity of the patient’s condition according to the SOFA and APACHE II scales (p <0.05). A sudden increase and persistence of a high IAP level for a long time in patients with closed abdominal trauma indicate the use of active surgical tactics to perform decompression. The decision to decompress the abdominal cavity is based on IAP monitoring, considering the clinical picture of developing multiple organ failure.
The main cause of death in closed abdominal trauma is the development of multiple organ failure [1,2,3,4,5,6]. Intra-abdominal hypertension (AHI) syndrome occupies an important place in the pathogenesis of multiple organ failure [7,8,9]. It is known that an increase in AHI contributes to an increase in the mortality rate, primarily in extremely severe patients [10]. The central link in the pathogenetic treatment of AHI syndrome is surgical aid. In connection with the above, this study analyzed the effect of various methods of surgical treatment on changes in the intra-abdominal pressure (IAP) in the postoperative period [11,12,13,14].
The ”gold standard” for indirect measurement of intra-abdominal hypertension is the use of the bladder. Since the wall of the bladder is well stretchable and elastic with a volume of no more than 25 ml, it acts as a passive membrane and shows intra-abdominal pressure until it is true [15,16,17,18].
The purpose of the study was the timely prediction of the development of AHI syndrome in patients with closed abdominal trauma.
Material and research methods: All patients with closed abdominal trauma underwent measurement of intra-abdominal pressure and abdominal perfusion pressure (APP), for which a urethral catheter connected to a water pressure gauge of the Waldman apparatus was used. In this case, the IAP was examined every 6 hours. The APP was calculated by subtracting the IAP from the mean arterial pressure (MAP). SBP was determined using the following formula: SBP = (2 * diastolic blood pressure + systolic blood pressure) / 3.
The World Society developed the classification system for the Study of Abdominal Compartment Syndrome for AHI. Classification of AHI by degrees is as follows:
Grade I: IAD 12-15 mm Hg.;
II degree: IAD 16-20 mm Hg.;
III degree: IAD 21-25 mm Hg.;
IV degree: IAD> 25 mm Hg.
A normal APD is 60 mmHg. or higher.
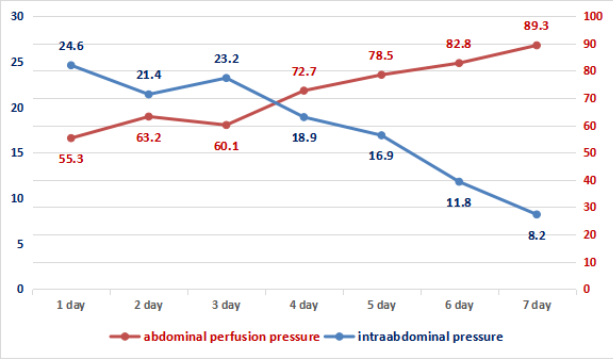
On the first day of the postoperative period, the patients of group I (traditional tactics, Figure 1) had a second-degree AHI with a critical increase in the level of intra-abdominal pressure by day 4 (20.9 \(\pm\) 3.8 mm Hg). At the same time, APD values remained low, reaching the minimum values (62.8 \(\pm\) 8.7 mm Hg) by day 3 of the postoperative period. In the dynamics against treatment background in the first week, in 58.7% of cases, there was a gradual decrease in IHD and normalization of APD indicators. In 94 (45.2%) patients, various complications developed (incompetence of the inner intestinal anastomosis, eventration of the abdominal organs, enclosed abscesses of the abdominal cavity), gastroduodenal bleeding, early adhesive obstruction), which were the reason for the reoperation.
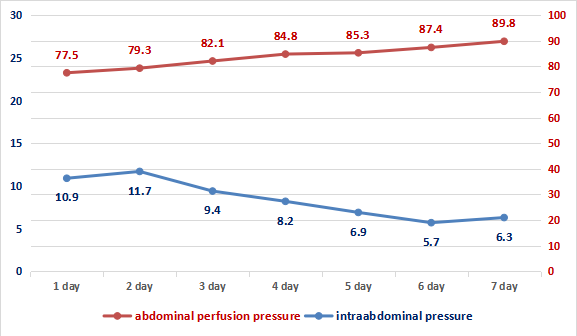
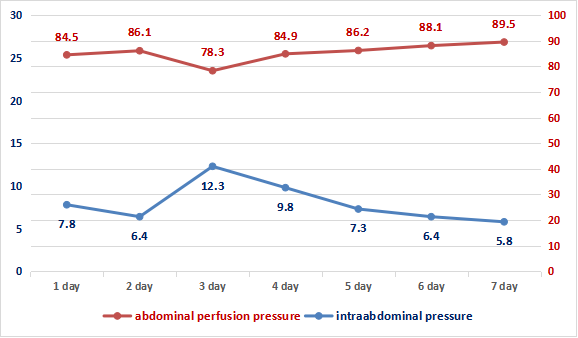
In subgroups IIa and IIb of groups (damage control surgery, Figures 2 and 3), a statistically significant decrease in IAP were observed on the initial day of the postoperative period: up to 10.9 \(\pm\) 7.8 mm Hg. Art. in subgroup IIa and up to 7.8 \(\pm\) 3.5 mm Hg. Art. in subgroup IIb (p> 0.05). There is an improvement in APD indicators – up to 77.5 \(\pm\) 5.8 mm Hg. Art. and 84.5 \(\pm\) 4.2 mm Hg. Art. respectively (p> 0.05), which shows an improvement in microcirculation processes in the main group’s victims. Moreover, the increase in IAP in the IIa subgroup of patients on the third day of the postoperative period to 12.3 \(\pm\) 3.7 mm Hg. Art. should not be misleading since this depends on the second stage of surgical tactics and the final closure of the surgical wound.
The frequency of the development of multiple organ failure according to the criteria and the assessment on the SOFA scale were compared on the second day of the postoperative period since it was during this period that the most significant difference in IAP indicators was revealed between I and IIa, and I and IIb groups (Table 1).
| Groups Systems | Group I, n = 208 | Subgroup IIa, n = 152 | Subgroup IIb, n = 87 |
|---|---|---|---|
| The cardiovascular system | 22.5\% * | 55.6% | 33.3% |
| urinary system | 45% * | 22.2% | 22.2% |
| Respiratory system | 85% | one hundre | 63.0% |
| Liver |
– |
– | |
| Coagulating system | 10% | 22.2% | 3.7% |
| Metabolic dysfunction | 32.5% * | 11.1% | 7.40% |
| CNS | 87.5% | 77.8% | 17.4% |
| SOFA, score | 7.3 \(\pm\) 1.8 * | 3.4 \(\pm\) 1.5 | 3.7 \(\pm\) 1.8 |
The high incidence of acute cerebral failure in all groups is explained by the nature of the trauma, that is, abdominal trauma was almost always combined with craniocerebral trauma, which was the cause of neurological deficit on the Glasgow coma scale. Manifestations of hepatic impairments were not observed in any of the cases, and impairments of the coagulating system were also rare and did not differ significantly among the groups. But nevertheless, in the first group there were significantly more patients with disorders in the cardiovascular, urinary, and metabolic disorders. This group of patients really needed more inotropic therapy. The result of the SOFA assessment showed a truly higher score in the severity of organ disorders in the first group.
The overall mortality rate in patients with abdominal injuries and associated severe trauma was 67.8%. The number of deaths among the patients of the first group was 119 out of 208 (57.21%), in the second group – 88 out of 270 (32.59%). Differences between IIa and IIb subgroups are not significant (p < 0.05). However, the differences in indicators I and IIa, I and IIb by subgroups are significant (\(p < 0.05\)).
Treatment results were studied in absolutely all patients with different IAP parameters during admission to the ICU. The average IAP in those patients who survived was 8.5 \(\pm\) 3.2 mm Hg, and in deceased patients – 24.2 \(\pm\) 1.8 mm Hg. (p < 0.05). But in this case, a natural dynamics of an increase in the mortality rate with an increase in IAP was noted.
When analyzing the relationship between AHI, APD, the frequency of multiple organ failure and the general severity of the condition of the victims, a statistically significant correlation was confirmed between the IAP and the severity of the patient’s condition according to the SOFA and APACHE II scales (\(p < 0.05\)). The increase in IAP level corresponded to the worsening of the severity of the condition of the victims according to the SOFA and APACHE II scales, which was confirmed by the progress of the clinical picture of multiple organ failure.