Aim: To assess various risk factors for development of CHD among patients. \Methodology: Seventy- eight patients of either sex were included. Various parameters such as age, gender, cardiac markers, family history, history of alcohol intake and smoking was recorded. Results: There were 32 patients >45 years of age and 46 below 45 years of age. Out of 78 patients, females were 27 and males were 51. It was found that 26 had primary education, 37 had secondary and 15 had higher education. 38 were employed and 40 were non- employed. 42 were married and 36 were unmarried. Family history was positive in 51 and negative in 26. 20 had hypertension, 36 had CHD and 22 had both HTN & CHD. 45 had habit of smoking, 47 had alcoholism and 40 had no physical activity. A significant difference was observed (P< 0.05). Conclusion: Common risk factors for CHD was obesity, hyperglycaemia, family history, high LDL- C, ALT level, smoking, alcoholism and lack of physical activity.
Coronary heart disease (CHD) is the leading cause of deaths among all CVDs. It is characterized by accumulation of plaque within coronary arteries known as atherosclerosis [1]. Approximately 8.9 million deaths universally occur due to CHD [2,3] The increase incidence of CHD in developing as well as developed countries may be due to inadequate and lack of better health services. CHD is regarded as major cause of mortality and morbidity among all age groups [4,5].
There are various risk factors for CHD such as smoking, poor socioeconomic status, alcoholism, elevated blood pressure, elevated serum total cholesterol and low-density lipoprotein cholesterol (LDL-C), low serum high-density lipoprotein cholesterol (HDL-C), diabetes mellitus, oral contraceptives, nutrition, stress, depression and advancing age. Physical inactivity i.e. Lack of exercise and obesity are major risk factors [6,7].
Hypertension patients is on top of all worldwide. Lifestyle modification is one of the components of HTN management. Studies reveal that regular physical activity provide protection against HTN [8]. A reduction of approximately 3.2 mm Hg systolic and 2.7 mm Hg diastolic blood pressure has been seen with regular physical activity. But poorly controlled HTN (systolic \(\geq\)180 mmHg and diastolic \(\geq\)100 mmHg), physical exercise should be deferred until their blood pressure stabilized [9].
Diet has major role in reducing systolic and diastolic blood pressure. Low intake of sodium, potassium, low dietary fats, intake of vegetables and fruits are best remedies for blood pressure control [10]. Foods with saturated fats, refined carbohydrates, low levels of fatty acids, processed foods, fast foods, and fried foods should be avoided [11]. Considering this, we attempted present study with the aim to assess various risk factors for development of CHD among patients of either sex.
A questionnaire was designed comprising information regarding age, gender, occupation, education, socio- economic status, history of smoking, alcohol intake, physical activity such as exercise for 30 minutes at-least 2 days a week, family history of hypertension or CHD etc. was recorded.
Measurement of weight (Kg) and height (cm) was done. Body mass index (BMI) was then calculated as BMI = weight (kg)/height (m2). BMI was categorized as underweight (< 18.5), normal (18.5-24.9), overweight (25.0-29.9) and obese (\(\geq\)30.0). Blood pressure monitoring was done using auscultatory method with the help of sphygmomanometer and stethoscope in upper left arm. Three reading at different interval by same operator was recorded and average was considered as final value. Seventh Joint National Committee criteria for classification of hypertension as normal (systolic < 120, diastolic < 80), pre-hypertension (systolic 120-139, diastolic 80-89), hypertension stage I (systolic 140-159, diastolic 90-99) and hypertension stage II (systolic \(\geq\)160 and diastolic \(\geq\)100) was followed.
10 ml of venous blood was taken for the estimation of plasma glucose, HLD-C, LDL-C, and ALT. Data were entered into Microsoft Excel 2019, then sorted and coded. Descriptive statistics were used to analyze the frequency and percentages. The analysis was done using SPSS version 20.0 (IBM). Results were calculated for significance (P 0.05) values.
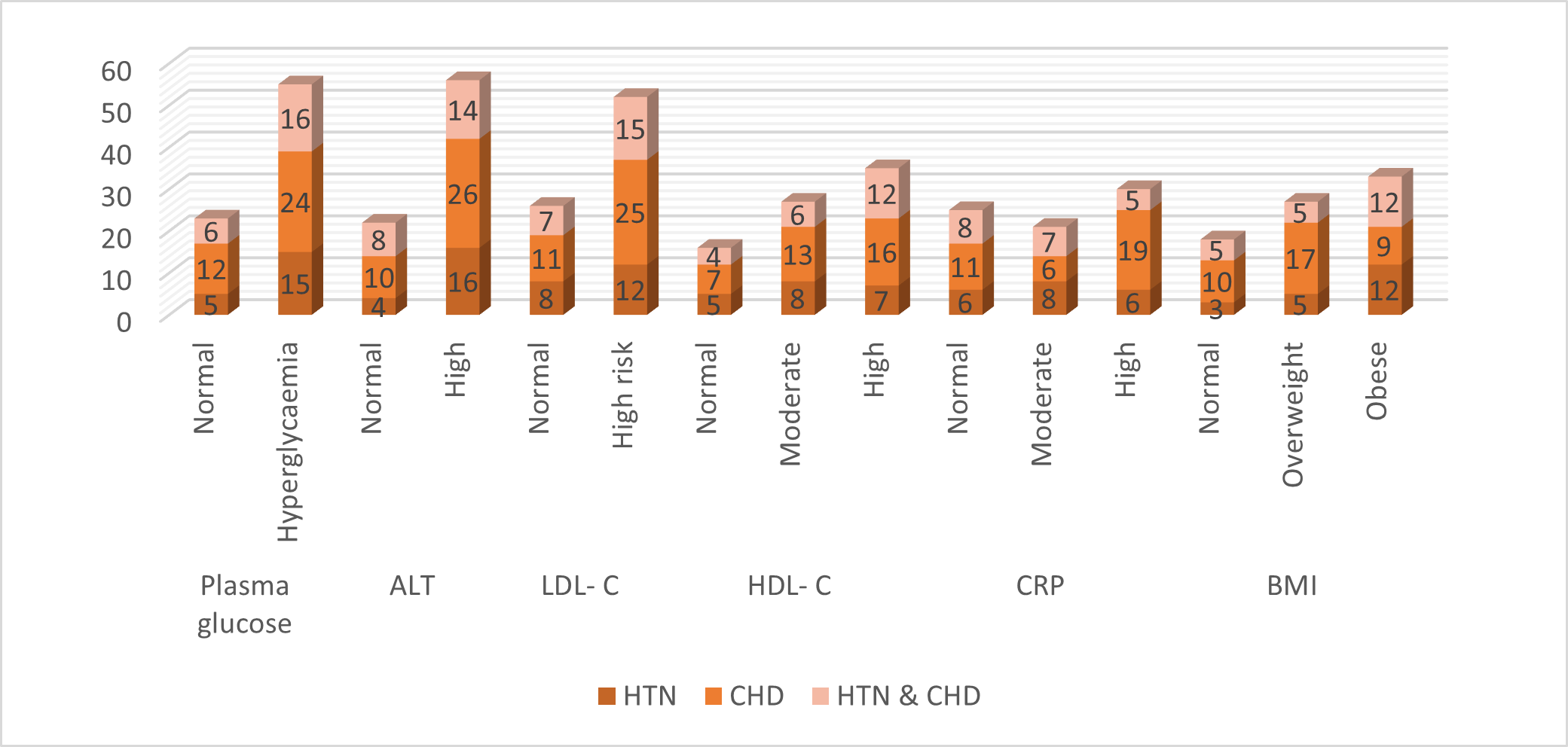
Among 20 hypertension patients, 15 had hyperglycaemia, among 36 CHD patients, 24 had hyperglycaemia and among 22 hypertension and CHD patients, 16 had hyperglycaemia. Riased ALT was seen among 16 HTN, 26 CHD and 16 CHD and HTN patients. LDL- C was high in 12, 25 and 15, HDL- C was high among 7, 16 and 12 HTN, CHD and CHD and HTN patients, CRP was high in 6, 19 and 5 HTN, CHD and CHD & HTN patients and BMI resulted obesity in 12, 9 and 12 HTN, CHD and CHD & HTN patients respectively \((P< 0.05)\) (Table 2, Figure 1).
| Variables | Number | P value |
|---|---|---|
| Age (years) | ||
| \textgreater{}45 | 32 | 0.05 |
| \textless{}45 | 46 | |
| Gender | ||
| Female | 27 | 0.05 |
| Male | 51 | |
| Education | ||
| Primary | 26 | 0.05 |
| Secondary | 37 | |
| Higher | 15 | |
| Occupation | ||
| Employed | 38 | 0.05 |
| Non- employed | 40 | |
| Marital status | ||
| Married | 42 | 0.05 |
| Unmarried | 36 | |
| Family history | ||
| Yes | 51 | 0.05 |
| No | 26 | |
| Disease type | ||
| Hypertension | 20 | 0.05 |
| CHD | 36 | |
| HTN \& CHD | 22 | |
| Smoking | ||
| Yes | 45 | 0.05 |
| No | 33 | |
| Alcohol intake | ||
| Yes | 47 | 0.05 |
| No | 31 | |
| Physical activity | ||
| Yes | 38 | 0.05 |
| No | 40 |
| Variables | Parameters | HTN (20) |
CHD (36) |
HTN & CHD (22) |
P value |
|---|---|---|---|---|---|
| Plasma glucose | Normal | 5 | 12 | 6 | 0.05 |
| Hyperglycaemia | 15 | 24 | 16 | ||
| ALT | Normal | 4 | 10 | 8 | 0.05 |
| High | 16 | 26 | 14 | ||
| LDL- C | Normal | 8 | 11 | 7 | 0.05 |
| High risk | 12 | 25 | 15 | ||
| HDL- C | Normal | 5 | 7 | 4 | 0.05 |
| Moderate | 8 | 13 | 6 | ||
| High | 7 | 16 | 12 | ||
| CRP | Normal | 6 | 11 | 8 | 0.05 |
| Moderate | 8 | 6 | 7 | ||
| High | 6 | 19 | 5 | ||
| BMI | Normal | 3 | 10 | 5 | 0.05 |
| Overweight | 5 | 17 | 5 | ||
| Obese | 12 | 9 | 12 |
Our study showed that 32 patients were above 45 years of age and 46 below 45 years of age. Out of 78 patients, females were 27 and males were 51. It was found that 26 had primary education, 37 had secondary and 15 had higher education. Roman et al., [17] found that of the 100 patients, 65% had hypertension, 23% had coronary heart diseases and 12% had both disease conditions. The most prevalent risk factors for hypertension and coronary heart diseases were: alcohol intake (67%), high blood pressure (59%), physical inactivity (61%), obesity (39%), alanine aminotransferase (43%), high-density lipoprotein (79%), low-density lipoprotein (65%), C-reactive protein (78%), sodium (41%) and potassium (40%). Moreover, age, plasma glucose, alanine aminotransferase, and C-reactive protein were found to be independently and positively associated with hypertension and coronary heart diseases.
It was seen that 38 were employed and 40 were non- employed. 42 were married and 36 were unmarried. Family history was positive in 51 and negative in 26. 20 had hypertension, 36 had CHD and 22 had both HTN & CHD. Hasan et al., [18] found that in patients with young CAD smoking was seen 29 patients (72.5%). Low HDL was found in 15 patients (37.5%), raised LDL was seen in 33 patients (82.5%), hypertension in 21 patients (52.5%), impaired fasting glucose / DM in 8 patients (20%). 27 patients (67.5%) had a positive family history of CAD. 20 patients (50%) were overweight, had BMI >30, 20 patients (50%) had STEMI. In that, 18 patients had AWMI (45%) and only 2(5%) had IWMI. 2(5%) had new onset LBBB. 11(27.5%) had NSTEMI and 7(17.5%) had Unstable angina. On echocardiography, 29 patients (72.5%) had LV dysfunction.
Our study demonstrated that among 20 hypertension patients, 15 had hyperglycaemia, among 36 CHD patients, 24 had hyperglycaemia and among 22 hypertension and CHD patients, 16 had hyperglycaemia. Hossain et al., [19] attempted to identify the factors that increase the risk for CHD as it is an extremely important area in health sciences. They also assessed overall risk. Logistic regression was used to model the log odds of developing CHD as a function of cholesterol category (0: < 190 mg/100 ml, 1: 190-219 mg/ml, 2: 220-249 mg/100ml), adjusting for age, sex and their interaction. The analysis showed that serum cholesterol level is a risk factor of coronary heart disease, but its effect is modified by the age category of the subjects. Sex is also associated with CHD, and moreover the effect of age on the 12-year incidence of CHD is gender-dependent.
It was observed that most of the hypertension, CHD and both hypertension and CHD patients had raised ALT, HDL- C, LDL- C, CRP and BMI. Kannel et al., [20] used data from the Framingham heart study to identify diabetes as a major cardiovascular risk factor. Based on 20 years of surveillance of the Framingham cohort, a two-fold to threefold increased risk of clinical atherosclerotic disease was reported. It was also one of the first studies to demonstrate the higher risk of CVD in women with diabetes compared to men with diabetes.
