This paper aims to compare 0.1% topical triamcinolone acetonide, oral methotrexate, and a combination of 0.1% topical triamcinolone acetonide and oral methotrexate in the management of oral lichen planus. 60 histologically confirmed cases of oral lichen planus were divided into 3 groups. Group T was given 0.1% topical triamcinolone acetonide, group M was given topical methotrexate and group C was given combination of both 0.1% topical triamcinolone acetonide and oral methotrexate. Clinical severity score and VAS was compared. The mean CSS at baseline was 5.4 in group T, 4.2 in group M and 4.1 in group C and at 4 months was 2.6 in group T, 2.1 in group M and 0.82 in group C. Baseline VAS was 6.5 in group T, 6.2 in group M and 7.1 in group C and at 4 months was 2.5 in group T, 1.3 in group M and 0.25 in group C. Group T had 3.2 years, group M had 3.1 years and group C had 3.3 years of duration of symptoms. It is concluded that the combination of triamcinolone and methotrexate exhibited maximum relieve of symptoms in patients with oral lichen planus.
Lichen planus is frequently occurring muco- cutaneous disease. It is one of the auto-immune inflammatory disease which has high impact on mental health of life. It is commonly occurring in females and middle age group is leading affected group [1]. It occurs in various forms such as reticular, bullous, erosive, erythematous, plaque, annular, papular etc [2,3,4]. It is one of the potentially malignant disorder in where chances of conversion to oral cancer is high [5]. Erosive form has high malignant potential [6]. The most striking oral feature of oral lichen planus is the presence of wickham striations. These are radiating greyish whitish striations commonly occur in buccal mucosa [7]. Other sites involved are lips, gingiva, soft palate etc. The predisposing factor for lichen planus is stress, depression, anxiety, psychiatric disorders [8].
Various treatment options are available for the management of lichen planus such as use of topical, systemic steroids, immunomodulators, herbal products etc [9]. Triamcinolone acetonide is one of the topical corticosteroids found to be effective in the management of oral lichen planus. Topical steroids is preferred over systemic steroids owing to its less side effects [10,11]. Methotrexate is one of the immunosuppressant drug inhibiting dihydrofolate reductase competitively, therefore hinder replication and function of T and B lymphocytes [12]. Its efficacy against cutaneous, oral erosive and vulvovaginal LP found be high [13]. Few studies have demonstrated equal effect of corticosteroids and methotrexate in oral lichen planus cases [14,15,16]. Considering this, this study was undertaken with the aim to compare 0.1% topical triamcinolone acetonide, oral methotrexate, and a combination of 0.1% topical triamcinolone acetonide and oral methotrexate in the management of oral lichen planus.
A computer-generated randomization of patients was done into 3 groups. Group T was given 0.1% topical triamcinolone acetonide, group M was given topical methotrexate and group C was given combination of both 0.1% topical triamcinolone acetonide and oral methotrexate. 0.1% topical triamcinolone acetonide was prescribed three times daily and methotrexate 0.3 mg/kg once/week. Patients were advised to continue the treatment for 4 months. Remission was defined absence of signs and symptoms of lesions. Live function test and complete blood count was determined. Clinical severity score was also calculated. The objective improvement was graded as excellent, good, poor, no response and worsening. Visual analog scale (VAS) was used for pain assessment. Results of the present study after recording all relevant data were subjected for statistical inferences using chi- square test. The level of significance was significant if p value is below 0.05 and highly significant if it is less than 0.01.
Group T had 3.2 years, group M had 3.1 years and group C had 3.3 years of duration of symptoms. A non- significant difference between groups was observed (P> 0.05) (Table 1).
| Parameters | Group T | Group M | Group C | P value |
|---|---|---|---|---|
| Duration of symptoms (years) | 3.2 | 3.1 | 3.3 | >0.05 |
| Difficulty in eating and/or drinking (%) | 85% | 90% | 94% | >0.05 |
It was observed that mean CSS at baseline was 5.4 in group T, 4.2 in group M and 4.1 in group C and at 4 months was 2.6 in group T, 2.1 in group M and 0.82 in group C. Baseline VAS was 6.5 in group T, 6.2 in group M and 7.1 in group C and at 4 months was 2.5 in group T, 1.3 in group M and 0.25 in group C. A significant difference between groups was observed (P< 0.05) (Table 2, Figures 1 and 2).
| Parameters | Group T | Group M | Group C | P value |
|---|---|---|---|---|
| Baseline CSS | 5.4 | 4.2 | 4.1 | >0.05 |
| 4 months CSS | 2.6 | 2.1 | 0.82 | >0.05 |
| Baseline VAS | 6.5 | 6.2 | 7.1 | >0.05 |
| 4 months VAS | 2.5 | 1.3 | 0.25 | >0.05 |
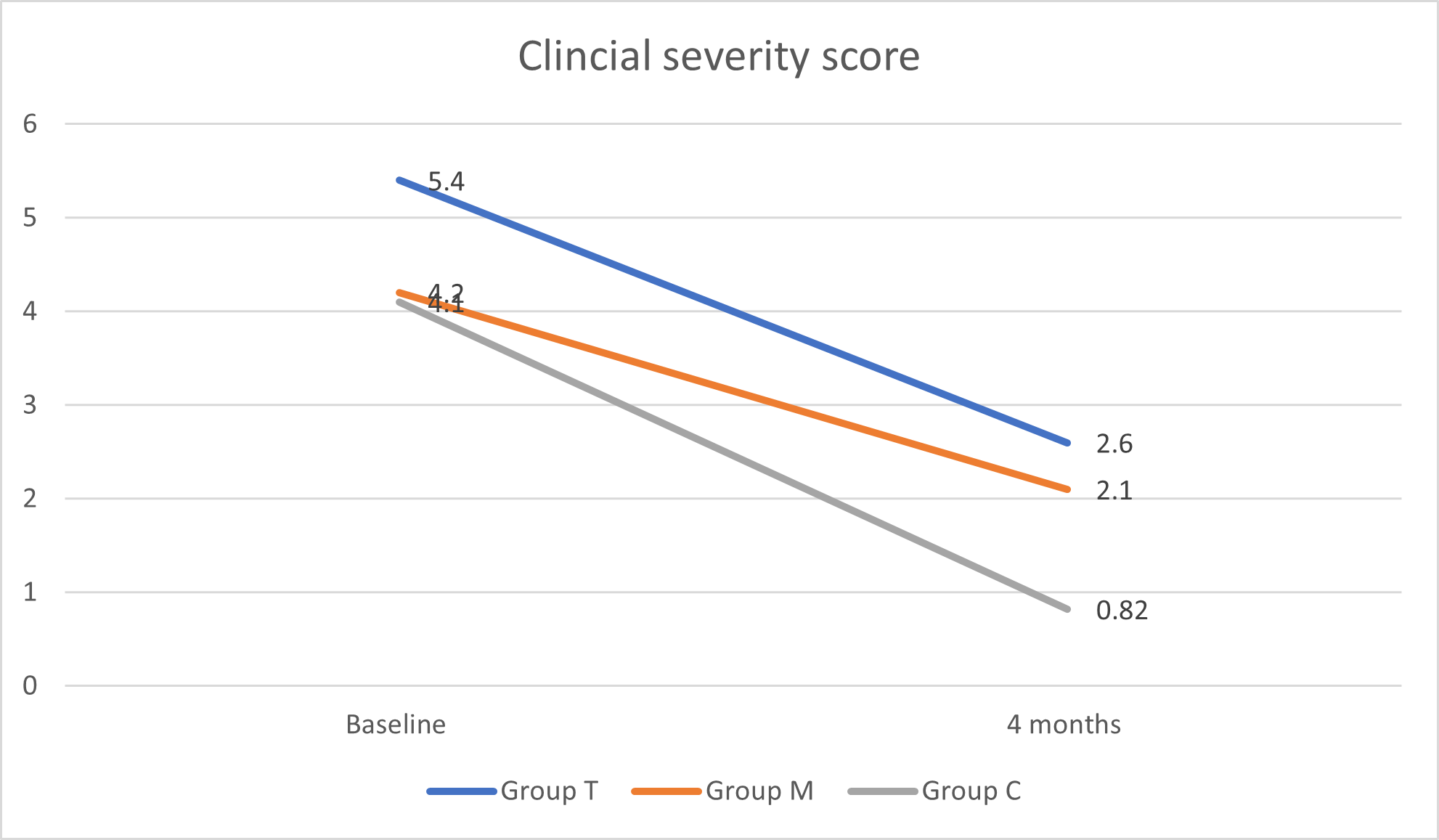
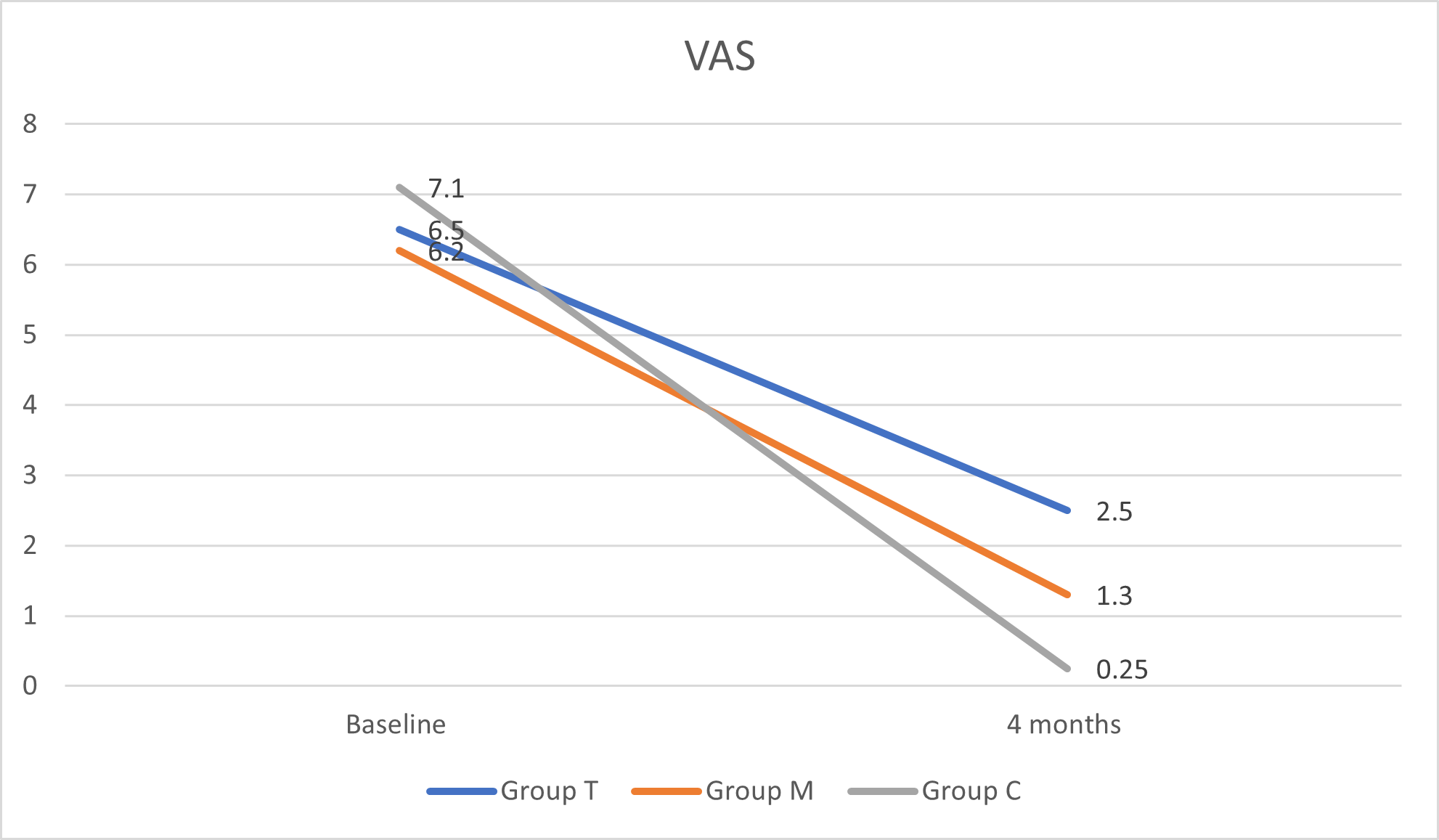
It was observed in our study that mean CSS at baseline was 5.4 in group T, 4.2 in group M and 4.1 in group C and at 4 months was 2.6 in group T, 2.1 in group M and 0.82 in group C. Baseline VAS was 6.5 in group T, 6.2 in group M and 7.1 in group C and at 4 months was 2.5 in group T, 1.3 in group M and 0.25 in group C. Malhotra et al., [18] involved 49 patients with moderate to severe oral lichen planus. Group A patients received either OMP comprising 5 mg of betamethasone orally on 2 consecutive days per week, group B received triamcinolone acetonide (0.1%) paste application thrice daily for 3 months. 23 of 25 patients in group A and 23 of 24 patients in group B completed the study. Good to excellent response was seen in 17 of 25 (68.0%) patients in group A as compared with 16 of 24 (66.0%) in group B at 6 months. Symptom-free state was achieved in 13 of 25 (52%) patients in group A and 12 of 24 (50%) in group B. The difference in the mean scores within each group was statistically significant from the fourth week onward in group A and eighth week onward in group B, whereas in patients with erosive disease it was second and twelfth week onward, respectively. Chamani et al., [19] compared effects of tacrolimus, clobetasol, and pimecrolimus on OLP and found that there was insufficient evidence to support superior efficacy of any specific treatment out of these three agents.
In our study in group C, combination of methotrexate and topical triamcinolone was significantly better than the other groups. This better result can be presumed to be due to the synergistic anti-inflammatory effects of methotrexate and triamcinolone as they seem to suppress inflammation via different pathways. Another advantage of this combination could be that topical corticosteroids help to reduce the dose of systemic therapy.
The term lichen planus was termed by Wilson in 1869. Cutaneous lesions typically present as small (2 mm) pruritic, white to violaceous flat-topped papules, which can increase in size to as much as 3 cm. Lichen planus patient usually manifests with burning sensation in oral cavity, the eating, speaking and drinking become difficult. Extreme painful condition make patient weak as ingestion become difficult. Reticular lichen planus is most common form occurs in 60-65% of cases. The interlacing striations give rise of red dot called stria of Wickham. Biopsy of the lesion reveal presence of colloid bodies, civatte bodies and hyaline bodies. Basal cell degeneration and saw tooth rete pegs are characteristic features [20]. The differential diagnosis should include lichenoid reactions, leukoplakia, squamous cell carcinoma, pemphigus, mucous membrane pemphigoid, and candidiasis. Lichenoid reactions in the oral cavity are invariably drug-induced lesions. The erosive or atrophic types that affect the gingiva should be differentiated from pemphigoid, as both may have a desquamative clinical appearance. Lupus erythematosus often has white plaque-like lesions with an erythematous border. In some cases, erythema multiforme can resemble bullous lichen planus, but it is more acute and generally involves the labial mucosa [21].
