Our main goal is to compare effect of ondansetron and ramosetron in attenuation of propofol-induced pain during induction of anaesthesia. A total of sixty subjects with American Society of Anesthesiologists (ASA) physical status (PS) 1 and 2, age ranging 18-60 years scheduled for various elective surgical procedures under general anaesthesia were included and were randomly divided into 2 groups. Group 1 received 4 mg of ondansetron and Group II received 0.3 mg of ramosetron. Mean age of patients in group 1 was 36.2 years and in group 2 was 36.0 years. There were 16 males and 14 females in group 1 and 17 males and 13 females in group 2. ASA grade I was seen in 20 in group 1 and 24 in group 2 and ASA grade II was seen in 10 in group 1 and 6 in group 2. A non- significant difference between both groups was seen (P> 0.05). Pain score 0 was observed in 14 in group 1 and 20 in group 2, score 1 in 9 in group 1 and 6 in group 2, score 2 in 4 in group 1 and 3 in group 2 and score 3 seen in 3 in group 1 and 1 in group 2. A significant difference between both groups was seen (P< 0.05). Ramosetron alone can be used to reduce the propofol-induced pain. Pre-treatment with IV ramosetron found to be effective as compared to ondansetron in preventing propofol-induced pain.
Propofol has attained unmatched popularity as an agent for intravenous (i.v.) induction. It is also used for short duration surgery, day care surgery, sedation and ambulatory surgery [1]. But very often, it has the disadvantage of causing pain or discomfort on injection, especially when given in small veins on the dorsum of hand [2,3]. This pain may be distressing to the patients and can reduce the acceptability of an otherwise useful agent [4]. Among 33 clinical problems, propofol-induced pain ranked seventh when both clinical importance and frequency were considered [5].
Propofol, a widely used drug for induction, often causes local pain when administered into a peripheral vein [6]. Many patients experience mild to moderate pain or even excruciating pain during propofol injection. Several methods have been described to reduce this pain, of which most effective and common are the use of a larger vein and mixing with lignocaine [7].
Numerous studies have been conducted to know the better among them for prevention of post-operative nausea and vomiting (PONV) but less for reducing propofol-induced pain. Ondansetron has been proved to have a local anaesthetic effect, other than antiemetic property [8]. There is no direct evidence for the increased local anaesthetic effect of ramosetron as compared to ondansetron [9]. However, ramosetron is benzimidazole derivative structurally independent of the previously developed 5-HT3 receptor antagonists such as ondansetron, granisetron and tropisetron [10]. Ramosetron is one of the potent 5-HT3 antagonist commonly used as an antiemetic and has been found to be effective in prevention of early PONV compared to ondansetron [11]. Considering this, we attempted present study with the aim to compare effect of ondansetron and ramosetron in attenuation of propofol-induced pain during induction of anaesthesia.
Patients were randomly divided into 2 groups based on computer-generated randomization. Group 1 received 4 mg of ondansetron and Group II received 0.3 mg of ramosetron. All the pre-treatment drugs were made into 2 ml volume with normal saline. After intravenous (IV) pre-treatment of study drug, manual occlusion of venous drainage was done at mid-arm with the help of an assistant for 1 min. This was followed by administration of propofol (1%) after release of venous occlusion. Pain was assessed with a four-point scale. Results were clubbed together entered in Excel sheet and statistically analyzed using Chi- square test. The level of significance was set below 0.05.
Mean age of patients in group 1 was 36.2 years and in group 2 was 36.0 years. There were 16 males and 14 females in group 1 and 17 males and 13 females in group 2. ASA grade I was seen in 20 in group 1 and 24 in group 2 and ASA grade II was seen in 10 in group 1 and 6 in group 2. A non- significant difference between both groups was seen (P> 0.05), see Table 1.
| Characteristics | Group 1 | Group 2 | P value |
|---|---|---|---|
| Mean age (Years) | 36.2 | 36.0 | >0.05 |
| Male: Female | 16:14 | 17:13 | >0.05 |
| ASA I | 20 | 24 | >0.05 |
| ASA II | 10 | 6 | < 0.05 |
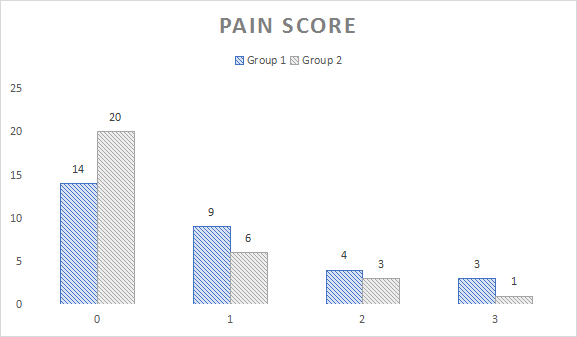
Pain score 0 was observed in 14 in group 1 and 20 in group 2, score 1 in 9 in group 1 and 6 in group 2, score 2 in 4 in group 1 and 3 in group 2 and score 3 seen in 3 in group 1 and 1 in group 2. A significant difference between both groups was seen (P< 0.05), see Table 2 and Figure 1.
| Pain score | Group 1 | Group 2 | P value |
|---|---|---|---|
| 0 | 14 | 20 | < 0.05 |
| 1 | 9 | 6 | < 0.05 |
| 2 | 4 | 3 | >0.05 |
| 3 | 3 | 1 | < 0.05 |
Our study comprised of 60 patients scheduled for various elective surgical procedures under general anaesthesia. Sumalatha et al., [15] in their study 150 adult patients posted for various elective surgical procedures under general anaesthesia were randomly assigned to three groups of 50 each. Group R received 0.3 mg of ramosetron, Group L received 0.5 mg/kg of 2% lignocaine and Group O received 4 mg of ondansetron. After intravenous (IV) pre-treatment of study drug, manual occlusion of venous drainage was done at mid-arm with the help of an assistant for 1 min. This was followed by administration of propofol (1%) after release of venous occlusion. Pain was assessed with a four-point scale. The overall incidence and intensity of pain were significantly less in Groups L and R compared to Group O (P = 0.001). The incidence of mild to moderate pain in Groups O, R and L was 56%, 26% and 20%, respectively. The incidence of score ‘0’ (no pain) was significantly higher in Group L (76%) and Group R (72%) than Group O (34%) (P < 0.001).
We observed that mean age of patients in group 1 was 36.2 years and in group 2 was 36.0 years. There were 16 males and 14 females in group 1 and 17 males and 13 females in group 2. ASA grade I was seen in 20 in group 1 and 24 in group 2 and ASA grade II was seen in 10 in group 1 and 6 in group 2. Lee et al., [16] in their study found that the incidence of pain was reported to be 60% and 38% respectively with pre-treatment by ramosetron 0.3 mg or combination with ramosetron and lignocaine 20 mg. In a study by Piper SN [17], severity but not the incidence of pain on injection was significantly reduced by dolasetron (50%) compared with placebo, and there was no significant difference between dolasetron and lignocaine. These results show effective reduction in propofol injection pain.
Our results showed that pain score 0 was observed in 14 in group 1 and 20 in group 2, score 1 in 9 in group 1 and 6 in group 2, score 2 in 4 in group 1 and 3 in group 2 and score 3 seen in 3 in group 1 and 1 in group 2. Ahmed et al., [18], the incidence of propofol injection pain was reduced from 60% to 15% after granisetron pre-treatment. The effect of pre- treatment by palonosetron (0.075 mg) on propofol-induced pain. 72.5% of patients experienced a decrease in the occurrence of propofol-induced pain. A study done by Swarika et al., [19] reported that ramosetron 0.3 mg IV was more effective than palonosetron 0.075 mg and ondansetron 8 mg in the early post-operative period.
Singh et al., [20] assessed the efficacy of pretreatment with various drugs to alleviate the propofol injection pain. One hundred American Society of Anesthesiology (ASA) I and II adults, scheduled for various elective surgical procedures under general anesthesia (GA), were included in the study. They were randomly divided into four groups having 25 patients in each group. Group A received pre-treatment with intravenous (i.v.) magnesium sulfate, group B received i.v. granisetron, group C received i.v. nitroglycerine and group D was the control group. One-fourth of the total calculated induction dose of propofol was administered over a period of 5 seconds. The patients were asked about the pain on injection. The intensity of pain was assessed using verbal response. A score of 0-3 which corresponds to no, mild, moderate and severe pain was recorded. All the three drugs reduced the incidence and intensity of pain on propofol injection but the order of efficacy in attenuation of pain on the propofol injection was granisetron > nitroglycerine > magnesium sulfate > control.
