Aim: To compare tension band wire and circumferential wiring for patellar fractures. Materials & Methods: One hundred twenty adult patients in age ranged 18- 50 years of either gender was randomly divided into groups viz. group 1 treated with tension band wire and group 2 with circumferential wiring for patellar fractures. Reich and Rosenberg scale, rage of motion and complications were recorded in both groups and compared. Results: At 4 weeks in group 1 and group 2, restriction of last \(10^{0}- 20^{0}\) was seen in 24 and 27, restriction of \(20^0-50^0\) was seen in 14 and 13, restriction \(>50^0\) was observed in 22 and 20. At 8 weeks, no restriction was seen in 8 and 9, restriction of last \(10^0- 20^0\) was seen in 38 and 39, restriction of \(20^0-50^0\) was seen in 10 and 9, restriction >500 was seen in 4 and 3. At 12 weeks, no restriction was seen in 15 and 20, restriction of last \(10^0- 20^0\) was seen in 35 and 32, restriction of \(20^0-50^0\) was seen in 8 and 7 and restriction \(>50^0\) was seen in 2 and 1 in group 1 and 2 patients respectively. A significant difference was observed (P< 0.05). Conclusion: Both techniques for the management of patellar fractures were equally effective in achieving functional outcome.
The patella is the largest sesamoid bone; it is embedded in the quadriceps tendon, provides the mechanical advantage and leverage that increases the force of knee extension [1]. Tensile forces are transmitted from the quadriceps to the tibia via the patella, the patella is also subjected to compressive forces at the articulation with the femur [2].
Displaced patella fractures or those which disrupt the extensor mechanism are usually managed operatively. The current standard remains a tension band wire (TBW) construct, with the option of additional cerclage wiring or TBW through cannulated screws [3]. Elderly patients and particularly those with comminuted patella fracture are “difficult patella fractures” as their osteopenic bone often lacks the strength to support a TBW and/or cerclage, resulting in fixation failure prior to bone union [4]. Fractures of the patella may be treated conservatively or surgically. Conservative management may be ideal for the patient who is non-ambulatory, had a prior failed extensor mechanism, those with an ankylosed joint, or particular fracture characteristics [5]. Typically, this involves immobilization of the extremity in full extension with partial weight bearing for several weeks. If the injury is not amendable to conservative management, then surgical intervention is merited to mitigate disability [6]. However, surgical management of patellar fractures is complicated secondary to its various tendinous attachments, which serve as displacing vectors on fracture fragments making fracture alignment not easily amenable to fixation [7].
Of all surgical management of patellar fractures such as modified tension band wiring (TBW), cerclage wiring, screw fixation, plating, and partial or total patellectomy, cerclage wiring and TBW are popular [8]. Tension band wiring (TBW) technique, one of the most commonly used surgical methods in treating a tension fracture, has a sound biomechanical advantage such that it can convert a tensile force into a compressive force when the joint is brought through a range of motion [9]. Percutaneous cerclage wiring for patella fracture can be applied through several small skin incisions without dissecting the fractured region and surrounding soft tissues and provides a minimally invasive approach to this procedure [10]. Considering this, the present study was conducted with the aim to compare tension band wire and circumferential wiring for patellar fractures.
Group 1 had 32 males and 28 females and group 2 had 35 males and 25 females (Table 1).
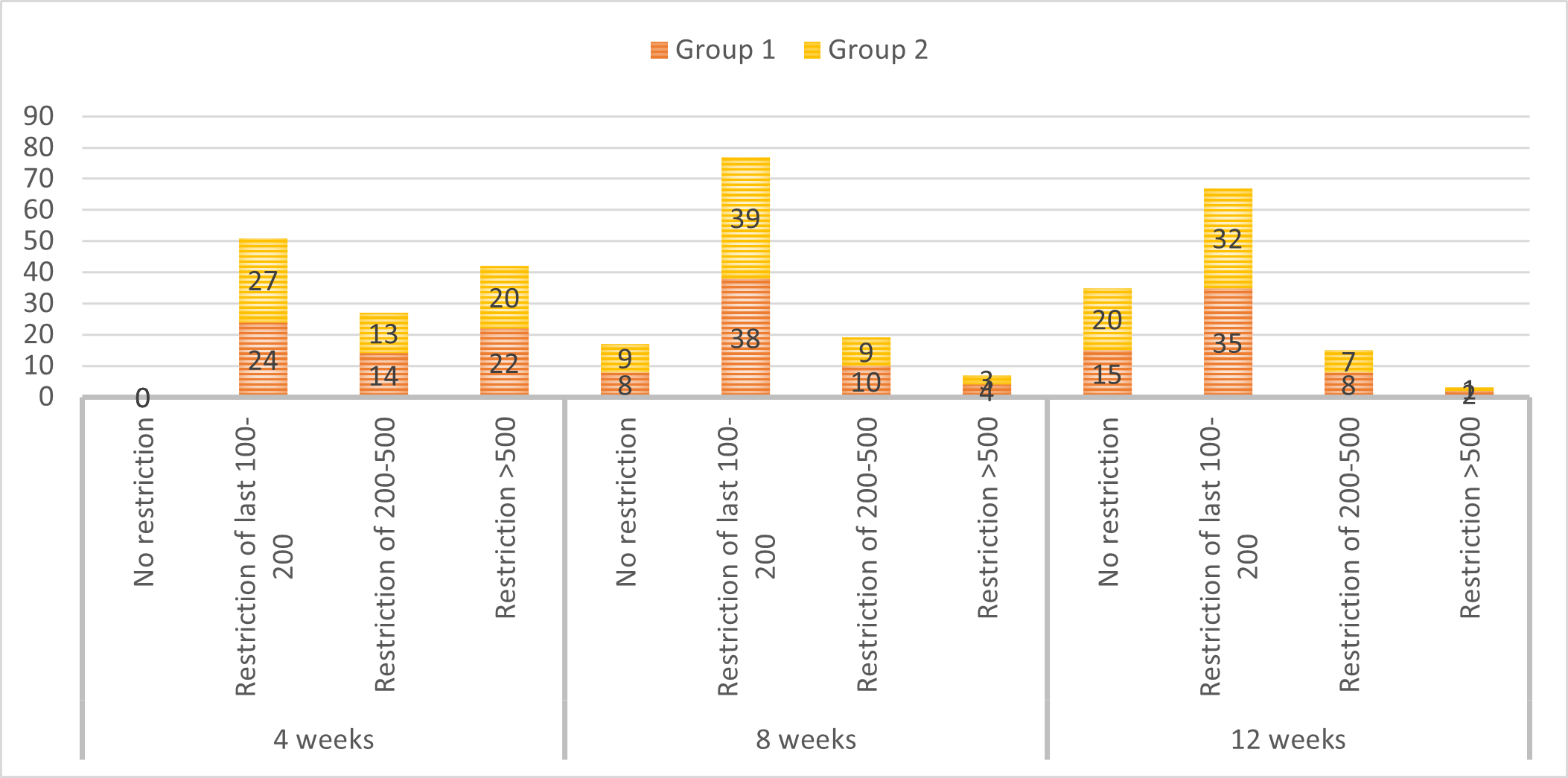
At 4 weeks in group 1 and group 2, restriction of last \(10^0- 20^0\) was seen in 24 and 27, restriction of \(20^0-50^0\) was seen in 14 and 13, restriction \(>50^0\) was observed in 22 and 20. At 8 weeks, no restriction was seen in 8 and 9, restriction of last \(10^0- 20^0\) was seen in 38 and 39, restriction of \(20^0-50^0\) was seen in 10 and 9, restriction \(>50^0\) was seen in 4 and 3. At 12 weeks, no restriction was seen in 15 and 20, restriction of last \(10^0- 20^0\) was seen in 35 and 32, restriction of \(20^0-50^0\) was seen in 8 and 7 and restriction >500 was seen in 2 and 1 in group 1 and 2 patients respectively. A significant difference was observed \((P< 0.05)\) (Table 2, Figure 1).
| Duration | ROM | Group 1 | Group 2 | P value |
|---|---|---|---|---|
| 4 weeks | No restriction | 0 | 0 | 0.05 |
| Restriction of last 100- 200 | 24 | 27 | ||
| Restriction of 200-500 | 14 | 13 | ||
| Restriction >500 | 22 | 20 | ||
| 8 weeks | No restriction | 8 | 9 | 0.05 |
| Restriction of last 100- 200 | 38 | 39 | ||
| Restriction of 200-500 | 10 | 9 | ||
| Restriction >500 | 4 | 3 | ||
| 12 weeks | No restriction | 15 | 20 | 0.05 |
| Restriction of last 100- 200 | 35 | 32 | ||
| Restriction of 200-500 | 8 | 7 | ||
| Restriction >500 | 2 | 1 |
| Results | Group 1 | Group 2 | P value |
|---|---|---|---|
| Excellent | 20 | 22 | 0.05 |
| Good | 32 | 30 | |
| Fair | 5 | 7 | |
| Poor | 3 | 1 |
Results were excellent in 20 in group 1 and 22 in group 2, good in 32 in group 1 and 30 in group 2, fair in 5 in group 1 and 7 in group 2 and poor in 3 in group 1 and 1 in group 2. A non- significant difference was observed (P> 0.05) (Table 3).
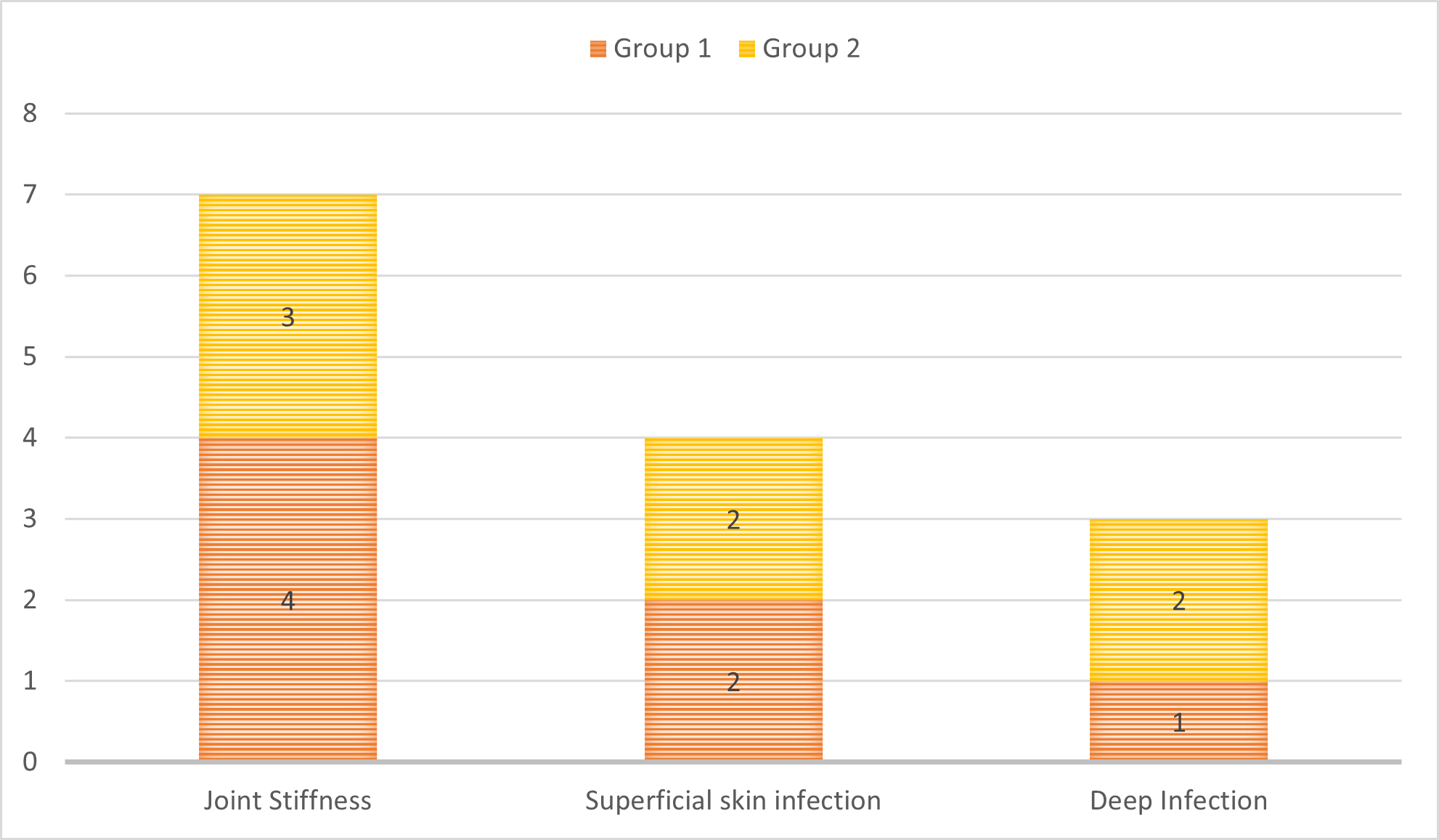
Joint stiffness was seen in 4 in group 1 and 3 in group 2, superficial skin infection was seen in 2 in each group and deep infection 1 in group 1 and 2 in group 2. A non- significant difference was observed (P> 0.05) (Table 4, Figure 2).
| Complications | Group 1 | Group 2 | P value |
|---|---|---|---|
| Joint Stiffness | 4 | 3 | 0.05 |
| Superficial skin infection | 2 | 2 | |
| Deep Infection | 1 | 2 |
Our results showed that group 1 had 32 males and 28 females and group 2 had 35 males and 25 females. Asimuddin et al., [16] in their study clinical and radiological investigations were carried out. Patients underwent Tension Band Wiring or Circumferential Wiring for the sustained fracture. Patients were followed up at 4 weeks, 8 weeks, 12 weeks till fracture union and once at 1 year after surgery using Reich and Rosenberg criteria. There was no significant difference regarding the mean age, gender, and mechanism of the fractures in patients treated by two methods of TBW and CW. 1 case of superficial infection and 3 cases of joint stiffness were noted after CW and 1 case of superficial infection and 2 cases of joint stiffness had occurred after TBW. 60% excellent, 25% good, 5% fair and 10% poor results were observed after Circumferential Wiring and 65% excellent, 15% good, 15% fair and 5% poor results after TBW. Patients of both groups showed an appreciable and statistically significant improvement in functional outcome at 3 months follow-up period as evidenced by Reich and Rosenberg Criteria that reveals no major difference. Furthermore, the difference in improvement between the two groups was not statistically significant at 3 months.
We observed that at 4 weeks in group 1 and group 2, restriction of last \(10^0- 20^0\) was seen in 24 and 27, restriction of \(20^0-50^0\) was seen in 14 and 13, restriction \(>50^0\) was observed in 22 and 20. At 8 weeks, no restriction was seen in 8 and 9, restriction of last \(10^0- 20^0\) was seen in 38 and 39, restriction of \(20^0-50^0\) was seen in 10 and 9, restriction \(>50^0\) was seen in 4 and 3. At 12 weeks, no restriction was seen in 15 and 20, restriction of last \(10^0- 20^0\) was seen in 35 and 32, restriction of \(20^0-50^0\) was seen in 8 and 7 and restriction \(>50^0\) was seen in 2 and 1 in group 1 and 2 patients respectively. We observed that results were excellent in 20 in group 1 and 22 in group 2, good in 32 in group 1 and 30 in group 2, fair in 5 in group 1 and 7 in group 2 and poor in 3 in group 1 and 1 in group 2. Our results demonstrated that joint stiffness was seen in 4 in group 1 and 3 in group 2, superficial skin infection was seen in 2 in each group and deep infection 1 in group 1 and 2 in group 2. Passias et al., [17] reviewed the multiple different patella fixation strategies and to evaluate the outcomes and complications associated with each. One hundred and fifteen patients who underwent patellar fracture fixation at an urban Level I-Trauma center were retrospectively reviewed. Operative treatment included open reduction and internal fixation with plate and screw devices, tension band wiring (TBW), cannulated screw tension band wiring (CS-TBW), isolated interfragmentary screw fixation, or partial patellectomy with soft tissue repair and tendon advancement. Patient demographics, fracture and injury characteristics, operative variables, radiographic information, and post-operative outcome measurements were recorded for each patient assessed in the study. Results demonstrated that plating techniques had the highest overall rate of union. Furthermore, a significant decrease in implant removal with utilization of isolated suture/wire was appreciated compared to other fixation groups \((p< 0.01)\).
