Aims: Mucormycosis is an acute invasive fungal infection which is rare, opportunistic and can potentially cause fatal complications. This study aimed to evaluate demographic data, disease presentation, medical &/or topical, surgical treatment.
Material and methods: Total twenty five patients with mucormycosis treated at tertiary care hospital in Gujarat during three months duration from May to July 2021. After detailed history thorough Ear, Nose and throat examination was performed. Along with local examination, ophthalmologic and neurologic examination performed in every case. After Functional endoscopic sinus surgery, tissue sent for histopathologic examination.
Results: Twenty five patients diagnosed with Mucormycosis, 18(72%) patients were males and 7(28%) were females. All 25(100%) had past history of COVID 19 infection and Diabetes Mellitus. Out of 25, 23(92%) patients were treated with intravenous or oral steroids and 2(8%) patients were not treated with any steroids. MRI paranasal sinuses with orbit with brain cuts performed for all 25 patients after suspicion of mucormycosis. 12(48%) patients had Sinonasal involvement, 11(44%) were Rhino-orbital involvement, and 2(8%) had Rhino palatal involvement. All 25(100%) patients were given Injection Amphotericin B for 3-4 weeks according to response. 6(24%) Patients were also given Oral Posaconazole. We performed Functional endoscopic sinus surgery in 23(92%) patients. In two (8%) cases Sinus surgery performed along with Maxillectomy. All 25(100%) cases on histopathology confirmed of Mucormycosis.
Conclusion: Prognostic factors we observed in our study were involvement of rhino-orbito-cerebral disease shows poor prognosis. Good Diabetes control showed early recovery. Early identification and early treatment improves prognosis as well as survival rates.
Sinonasal mucormycosis is an acute invasive fungal infection which is rare, opportunistic and potentially fatal, that mostly occurs in immunocompromised patients[1]. Such immunocompromised patients are those with diabetes mellitus, prolonged corticosteroid therapy, solid organ transplant recipients, neutropenia and haematological malignancies[2]. Coronavirus disease (COVID-19), attributed to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was declared a global pandemic by the World Health Organisation(WHO) in March 2020[3].
In recent years, it was observed a surge regarding the incidence of mucormycosis infection; extracted evidence from multiple published epidemiological studies revealed a pooled prevalence of Coronavirus disease 2019 (COVID-19)-associated mucormycosis 50 times higher than before the pandemic era.The proposed mechanism of pathogenesis consists of inhalation of fungal spores from air that determine the colonization of respiratory mucosa at the level of the nasal cavity and paranasal sinuses and rapid spread to surround-ing structures, facilitated by its angio-invasive properties.Based on the anatomical region where mucormycosis has developed, it can be classified into rhino-orbito-cerebral, gastrointestinal, pulmonary, renal, cutaneous, disseminated. Other rare sites include ear, parotid gland, heart, lymph nodes, and bones.
This disease is caused by saprophytic and opportunistic fungi of class Phycomycetes, order mucorales, family mucoraceae belonging to genus mucor and rhizopus[4]. The fungus is angioinvasive and causes thrombosis of vessels, with consequent black necrosis of nasal and sinus tissue. Surgery, antifungals- intravenous along with topical therapy remains the main treatment options.
Untreated of severe cases of Mucormycosis can lead to cavernous sinus thrombosis, periorbital destruction, palatine ulcers, osteomyelitis, disseminated infection and eventually death.
Total twenty eight patients with suspected mucormycosis treated at tertiary care hospital in Gujarat during three months duration from May to July 2021. Out of which total 25 cases has been included in this study. Two patients died due to complications related to COVID 19 infection and also complications of mucormycosis, of these one patient had histopathologically proven Rhino-orbito-cerebral mucormycosis and other had radiologically suspected Pulmonary mucormycosis. Third patient had radiologically suspected Sinonasal mucormycosis but clinically and histopathologically turn out to be negative, so patient treated as Rhinosinusitis case.
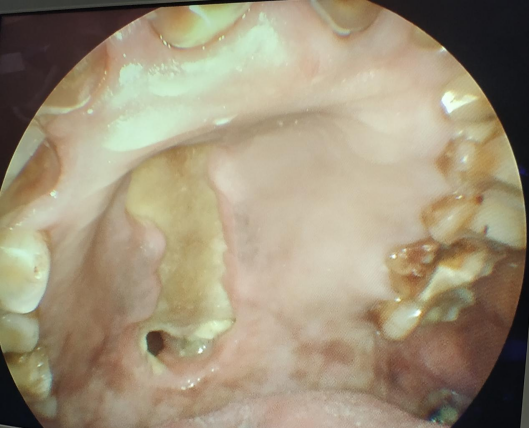
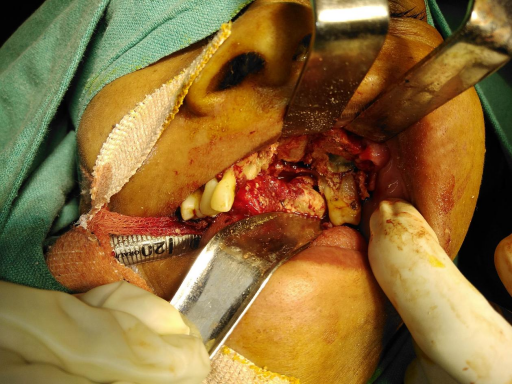
So, after excluding above mentioned three cases, in this study total 25 patients were analysed. After detailed history thorough Ear, Nose and throat examination was performed. All patients were also evaluated by ophthalmologists and Infectious disease specialist. Along with local examination, ophthalmologic and neurologic examination performed in every case. All routine blood investigations were done, see Figures 1,2 and 3.

| Comorbidity | Male | Females | Total |
|---|---|---|---|
| Diabetes | 18 | 7 | 25 (100%) |
| Hypertension | 5 | 4 | 9 (36%) |
| Symptoms : | Patient No. (%) |
|---|---|
| Nasal Obstruction | 22 (88%) |
| Nasal Discharge | 2 (8%) |
| Facial Pain | 18 (72%) |
| Facial Swelling | 5 (20%) |
| Vision Loss | 1 (4%) |
| Headache | 21 (84%) |
| Toothache | 2 (8%) |
| Periorbital Edema | 7 (28%) |
| MRI fnding | Patient No. (%) |
|---|---|
| Sinonasal | 12 (48%) |
| Rhino Orbital | 11 ( 44%) |
| Rhino Palatal | 2 (8%) |
| Surgical : | Patient No. (%) |
|---|---|
| FESS | 23 (92%) |
| FESS + locally kept Amphotericin soaked gelfoam | 5(20%) |
| FESS + Maxillectomy | 2 (8%) |
| FESS + Retrobulbar Amphotericin Inj. | 5 (20%) |
| Medical: | Patient No. (%) |
|---|---|
| Inj Amphotericin B | 25 (100%) |
| Oral Posaconazle | 6 (24%) |
| i. | Better penetration of Antifungal medications |
|---|---|
| ii. | Slows down disease progression and restricts the extent allowing time for bone marrow regeneration |
| iii. | Reduces the fungal load which reduces load on recovering neutrophils |
| iv. | Provides a specimen for histopathology |
Along with increase in the novel coronavirus (COVID – 19) cases, number of opportunistic fungal infections appears to be raised. Globally, several cases of mucormycosis have been observed in patients with COVID-19, the term being used is COVID-19 associated mucormycosis (CAM). Mucormycosis has been declared an epidemic in several Indian states and has been classified as a notifiable disease. Early diagnosis and prompt initiation of treatment is crucial as the condition can progress rapidly with fatal outcome. The etiology of the sudden rise of mucormycosis in India appears to be multifactorial in nature with several hypothesis linking mucormycosis to severe Covid-19 patients who are immune compromised and/or have associated co-morbidities. For example, diabetes, which is a known risk factor for Covid, is also found to be strongly associated with risk of mucormycosis. According to the WHO[5], about 1.5 million deaths were attributed to diabetes globally, and its prevalence is increasing rapidly in low- and middle-income countries. India, home to over 77 million diabetics, has the second highest number of diabetics in the world next to China[6] and that the prevalence of diabetes in India is on the rapid rise[7].
In our study majority of patients were a male, which is similar to study by Pal et al.,[8]. We observed that all our cases were related to COVID-19 infection, majority of patients had suffered from disease. So Mucormycosis linked with it. Our all cases had associated diabetes mellitus, observed in all 25(100%) cases. Hyperglycemia, as seen in patients with uncontrolled diabetes mellitus, leads to phagocyte dysfunction, impaired chemotaxis and defective intracellular killing by oxidative and non-oxidative mechanisms[9]. Although data on the degree of glycemic control were infrequently reported across all the included studies, it is expected that COVID-19 might have further worsened the glucose profile of the patients with diabetes, thereby further predisposing them to mucormycosis. SARS-CoV-2 can infect and replicate in the human islet cells, leading to $\beta$-cell damage and reduced endogenous insulin secretion. Besides, the plethora of cytokines, as seen in patients with COVID-19, can lead to worsening of insulin resistance.% with COVID-19, can lead to worsening of insulin resistance.
Usually elevated in patients with severe COVID-19, interleukin-6 (IL-6) causes insulin resistance by impairing the phosphorylation of insulin receptor and insulin receptor substrate-1[10].
The use of glucocorticoids is a known risk factor for the development of mucormycosis[11]. Glucocorticoid-induced immunosuppression, hyperglycaemia and lymphopenia predispose to the pathogenesis of mucormycosis. The rampant use of glucocorticoids in patients with COVID-19 has undoubtedly contributed to the upsurge in the number of cases of CAM. Another indirect association between the concomitant surge in COVID-19 and mucormycosis is the dissemination of fungal spores via water used in oxygen humidifiers. Indeed, hospital water is a potential reservoir for fungi including Mucorales[12]. After such study found, in our hospital we used distilled water in oxygen humidifiers in COVID affected patients. We could not find out its actual relation in occurrence of post COVID-19 mucormycosis, due to lack of proper follow up of cases that were treated with only oxygen therapy for COVID 19 infections.
The 1950 Smith and Krichner criteria[13] for the clinical diagnosis of mucormycosis are still considered to be gold standard and include: \begin{description}
In our study 12(48%) patients had Sinonasal involvement, 11(44%) had Rhino-orbital involvement, and 2(8%) had Rhino palatal involvement. These findings are similar to study by Abha et al.,[15], where most common sino-nasal disease involvement followed by rhino-orbital disease. In all our cases we performed Functional endoscopic sinus surgery. Advantages described in Table \ref{tab5}. In case of palatal involvement, after maxillectomy obturator was given to cover defect & to prevent nasal regurgitation.
Despite recent tremendous advancements in sinus surgery, invasive fungal sinusitis still has a high mortality rate. So, many researchers have recommended sinus surgery/debridement and long-term antifungal treatment. These might cause severe morbidity and complications, so some treatment techniques have been modified in order to gain better clinical outcomes. Direct introduction of amphotericin B to the sinus cavity is one of the options which we followed. We did it in 5(20%) cases, which showed better outcome. Those patients had early recovery. After surgery, local area packed with gelfoam soaked in Amphotericin B(50mg vial of Amphotericin B diluted in 10ml of sterile water). This method helps in reducing density of fungal spores. Many researchers have used topical treatment, but well designed, controlled studies are needed to evaluate patients responses to this type of treatment.
All 25 patients treated with Injectable Amphotericin B, with dose of 1 mg/kg/day or Liposomal Amphotericin B 3-5mg/kg/day for 2-3 weeks. Liposomal or conventional injection usage, decided on basis of availability, cost and comorbidities of patients. Amphotericin B acts by binding to ergosterol in the cell membrane of fungi. After binding with ergosterol, it causes the formation of ion channels leading to loss of protons and monovalent cations, which results in depolarization and concentration-dependent cell killing. Additionally, amphotericin B also produces oxidative damage to the cells with the formation of free radicals and subsequently increased membrane permeability. Amphotericin B also has a stimulatory effect on phagocytic cells, which assists in fungal infection clearance.The half-life of amphotericin B is from 24 hours to 15 days.
Infusion related reactions occur in few cases. Such reactions can be rigor, chills, fever, headache, nausea, malaise or generalised rashes. Reactions can be avoided or minimized by premedication with aspirin or ibuprofen or by adding 25mg of hydrocortisone to the infusion directly[13]. We did not notice any kind of infusion related reactions in our patients receiving Injection Amphotericin B. Oral Posaconazole(800mg per day) can be used for salvage treatment in patients who are intolerant to Amphotericin B. It can also be used as a step down therapy after initial control of the disease with Amphotericin B. We used oral Posaconazole in 6(24%) cases after initial control with Injection Amphotericin B. Oral Isavuconazole also being better option, but not used in any case due to unavailability.
Hyperbaric oxygen has been used as an adjunct to the current therapeutic approach of aggressive surgical debridement, Amphotericin B therapy and control of underlying predisposing conditions. Although studies have shown that hyperbaric oxygen exerts a fungistatic effect, its most important effect is to aid neovascularization with subsequent healing in poorly perfused acidotic and hypoxicbut viable tissue. Hyperbaric oxygen therapy for mucormycosis should consist of exposure to 100% oxygen for 90 min to 2 hour at pressures of 2.0-2.5 atmospheres with one or two exposures daily for a total of 40 treatments. Reported toxicities of hyperbaric oxygen include teratogenicity and, rarely, pulmonary or CNS side-effects. Although hyperbaric oxygen is offered by only a few medical facilities, it may be warranted in patients who appear to be deteriorating despite maximal surgical and medical therapy[16]. Though we did not treat any case of mucormycosis with Hyperbaric oxygen therapy.
Antifungal therapy started only after KOH or histopathological confirmed cases of Mucor. On histopathology, the fungal hyphae seen as broad, ribbon like, irregular and aseptate with branching at right angle. On KOH also broad, aseptate hyphae seen.
To note, our study has few limitations. 25 cases in this study can be considered as small sample size. This disease seen rarely in past but post COVID 19 era rapid surge was seen. High cost treatment is one of factor for less number of patients. Being an observational study there is no control group to evaluate differences.
