The article presents the results of studying the modern literature on diagnosing and treating severe concomitant abdominal trauma and their prediction. In addition, the authors provide the primary literature data of domestic and foreign authors in recent years.
Abdominal injuries account for 1.5 to 36.5% of peacetime injuries, but their frequency and severity continue to increase. According to A.N. Tulupov[1,2], in severe concomitant trauma, injuries to the abdominal organs are present in almost 30% of victims. Due to the severity of damage to internal organs and difficulties in diagnosis, such an injury is characterized by a high rate of complications and mortality, which, according to various authors, ranges from 25 to 65%. According to Shapot [3,4] and Afonina [5], with an isolated injury of one abdominal cavity, the lethality ranges from 5.1 to 20.4%, and with a combined injury – from 18.3 to 64% [6,7,8,9,10,11,12,13].
Closed abdominal injuries are accompanied by a large number of complications and high mortality due to difficulties in diagnosis and frequent combination with injuries to other organs, and systems [14,15,16,17,18,19,20,21]. A particular problem is the diagnosis and treatment of concomitant closed trauma of the abdominal organs, accompanied by shock. Hospital mortality in this variant of the pathology ranges from 17.3 to 72.7% [22,23,24,25,26]. For example, over the past five years, the mortality rate from road accidents in Russia has increased by 65%, and the death toll reaches 33-35 thousand people per year [27,28,29].
In the literature, several terms define multiple injuries to various areas of the body in severe trauma [30,31]. In the Russian literature, the term severe concomitant injury (TTS) is most often used. However, in the big medical encyclopedia [32] there is the following definition: polytrauma – simultaneous damage to several anatomical areas in one victim.
Concomitant injuries are simultaneous damage to several different systems or organs. TCT as a model of an extreme condition, is damage to two or more anatomical regions of the body. Concomitant injury, defined as the simultaneous injury of two or more of the body’s seven anatomical regions, is a complex multifactorial and severe type of injury characterized by numerous pathological syndromes, a frequent change in the dominant factor, a large number of complications, and a high mortality rate. In the diagnosis, the authors recommend indicating the leading injury. Thus, the analysis of scientific literature indicates that the choice of the volume of surgical intervention in patients with severe concomitant abdominal trauma against the background of traumatic and hemorrhagic shock is still an unsolved problem [33,34,35].
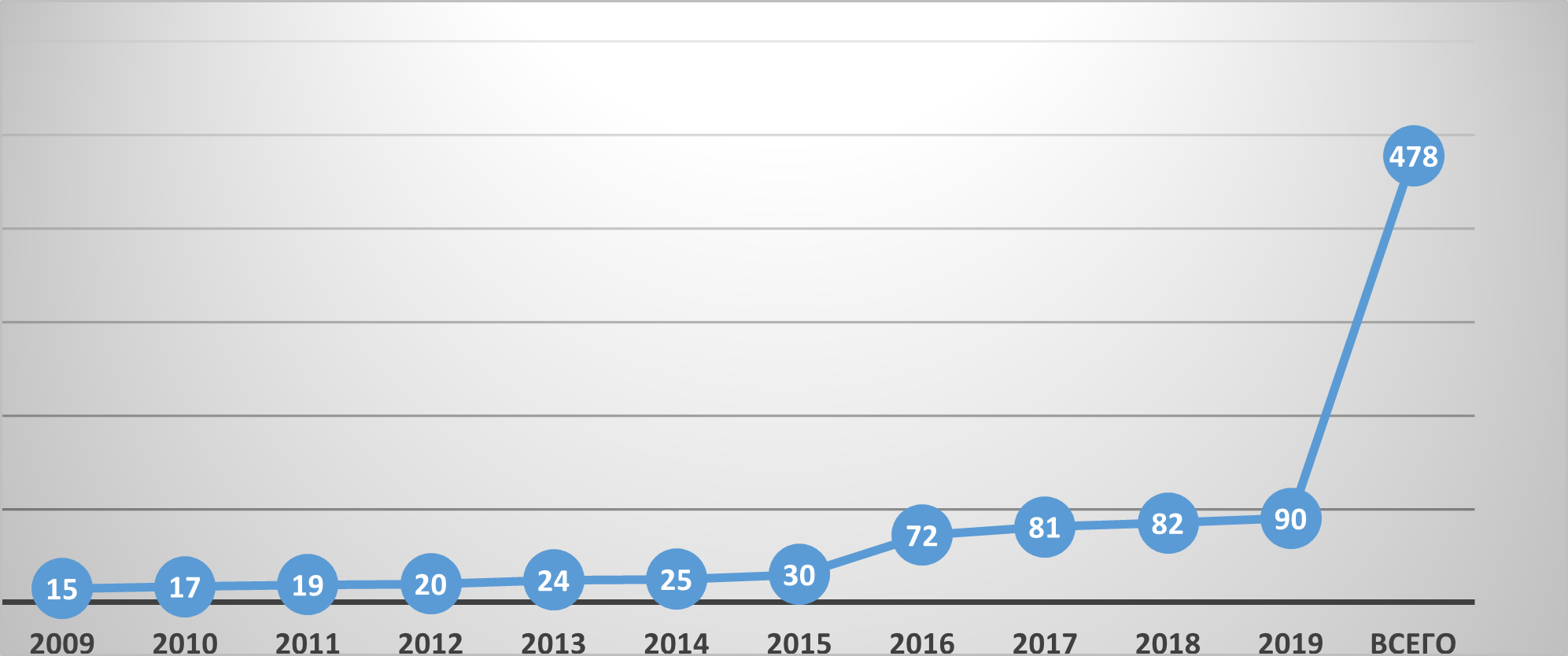
For the period from 2009-2019. Two thousand six hundred forty-five patients with concomitant trauma of the abdominal cavity and retroperitoneal space were admitted to the Samarkand branch of the RSCEMP, of which 447 (16.9%) patients were operated on with concomitant abdominal trauma.
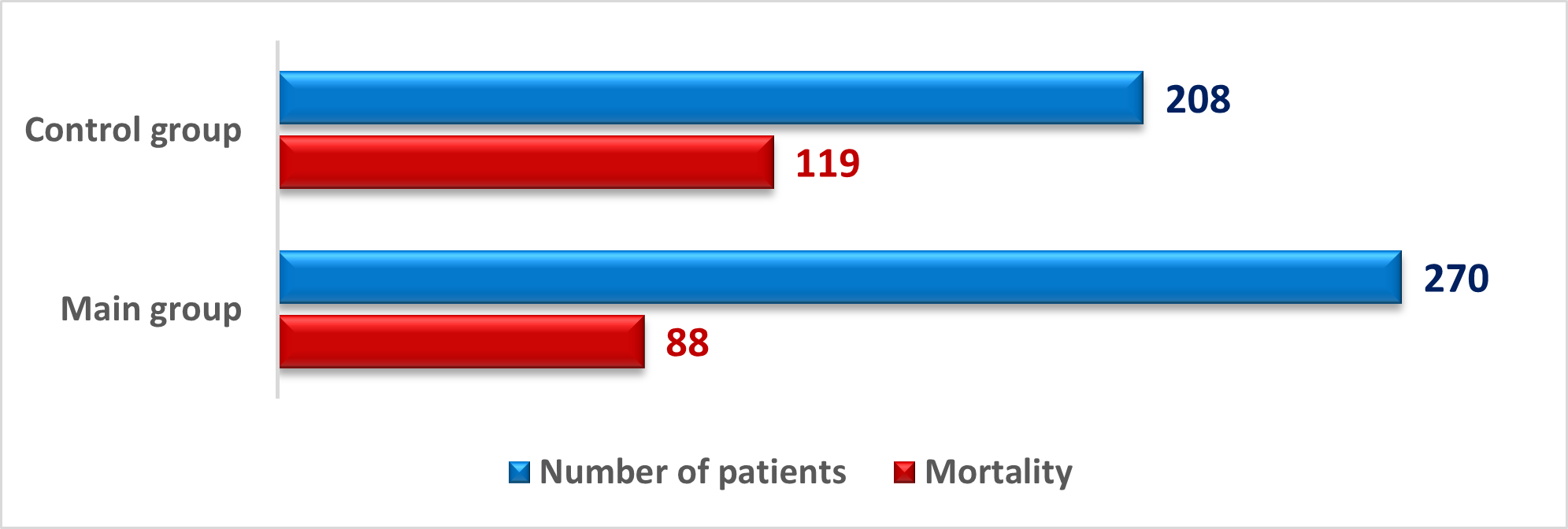
Our study consisted of two stages – a retrospective one based on the results of studying the case histories of 208 patients with shock-related mechanical trauma and a prospective one based on analyzing the treatment results of 270 critically ill patients hospitalized with concomitant trauma.
The criteria for inclusion in the research were the following attitudes: 1) shock-related concomitant mechanical trauma to the abdominal organs; 2) the age of the victims is from 18 to 89 years. The exclusion criteria were: 1) clinically significant comorbidities (oncological diseases and chronic diseases in the decompensated stage at the time of admission); 2) combined trauma of severe degree.
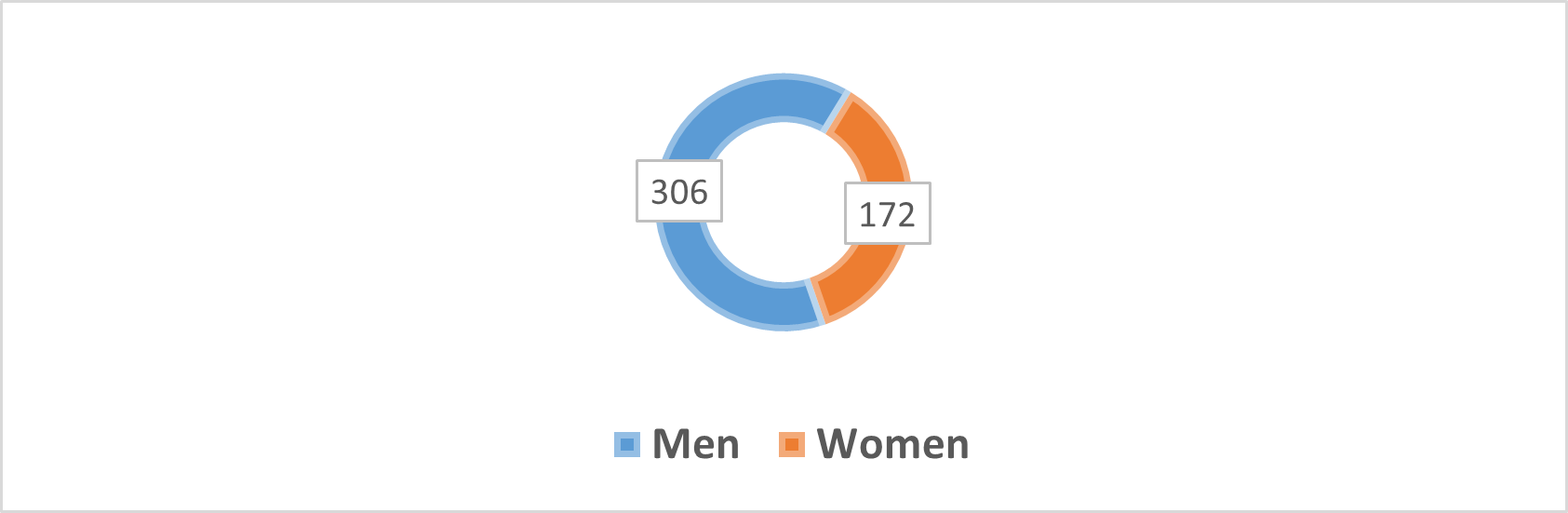
The study included 478 patients aged 18 to 89 years, among them – 306 men (64.0%) and 172 women (36.0%) – Figure 1.
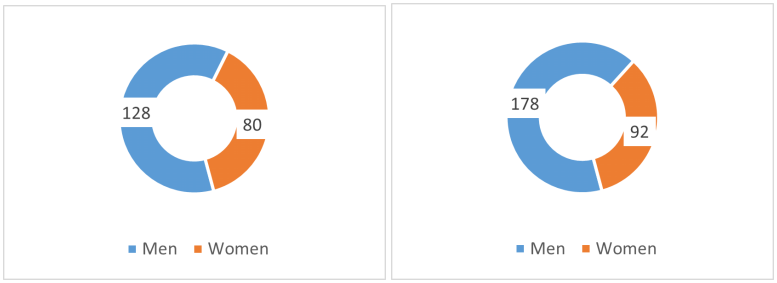
Sorting of victims with abdominal injuries in cases of combined trauma by gender in the control and main groups is illustrated in Figure 2.
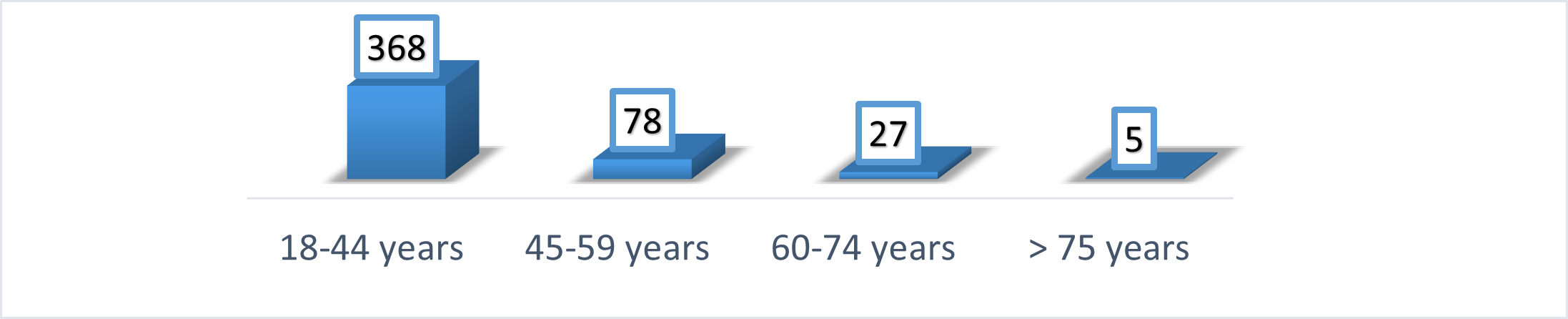
The average age of hospitalized patients was 33.8 \(\pm\) 13.4 years, and most of them were people of working age, which also emphasizes the relevance of the problem under study (Figure 3).
As seen in Figure 5, over ten years, the number of victims hospitalized in the SFRNCEMP increased six times. The overwhelming majority were delivered by ambulance teams – 416 (87%), who were provided with appropriate assistance at the scene of the accident to maintain the body’s vital functions and prevent the development of life-threatening conditions. However, 62 victims (13%) were admitted by gravity without providing the necessary assistance (Figure 4)

Among 478 victims, 447 (93.5%) were operated on. Of these, a lethal outcome was observed in the control group – out of 208 in 119 (57.21%), and in the main group – out of 270 – 88 (32.59%) – Figure 6. Thirty-one (11.48%) patients with abdominal injuries (liver in 25 and spleen in 6) underwent conservative therapy in the presence of concomitant injury.
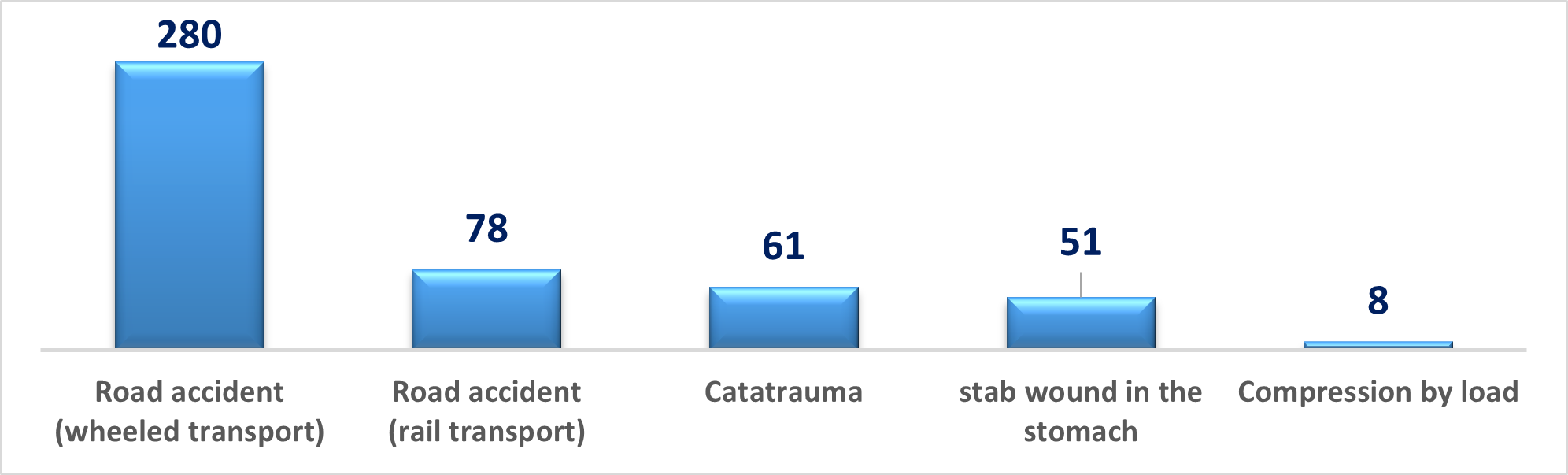
In most cases, the cause of injury was a road traffic accident (n = 358 – 74.89%), in 51 (10.67%) victims, the cause of injury was the result of striking the abdomen, in 61 (12.76%) catatrauma (Figure 7).
Alcohol intoxication was observed in 257 (53.77%) victims.
The severity of shock was assessed using the Algover-Gruber index (shock index).
Sorting of victims according to the degree of hemorrhagic shock is presented in Table 1. The data in the table indicate that 478 (100%) patients undergoing examination were admitted in a state of hemorrhagic shock (I, II, III and IV degrees).
| Index Algovera-Gruber | Shock degrees | Number of victims, n = 478 | Total died | ||
|---|---|---|---|---|---|
| I gr. | II gr. | I gr. | II gr. | ||
| Up to 1.0 | I | 101 | 5 | 15 | – |
| 1.0 to 1.5 | II | 20 | 60 | 18 | 10 |
| 1.5 to 2.0 | III | 31 | 164 | 30 | 57 |
| 2.1 and more | IV | 56 | 41 | 56 | 21 |
| Total | 208 | 270 | 119(57.21%) | 88(32.59%) | |
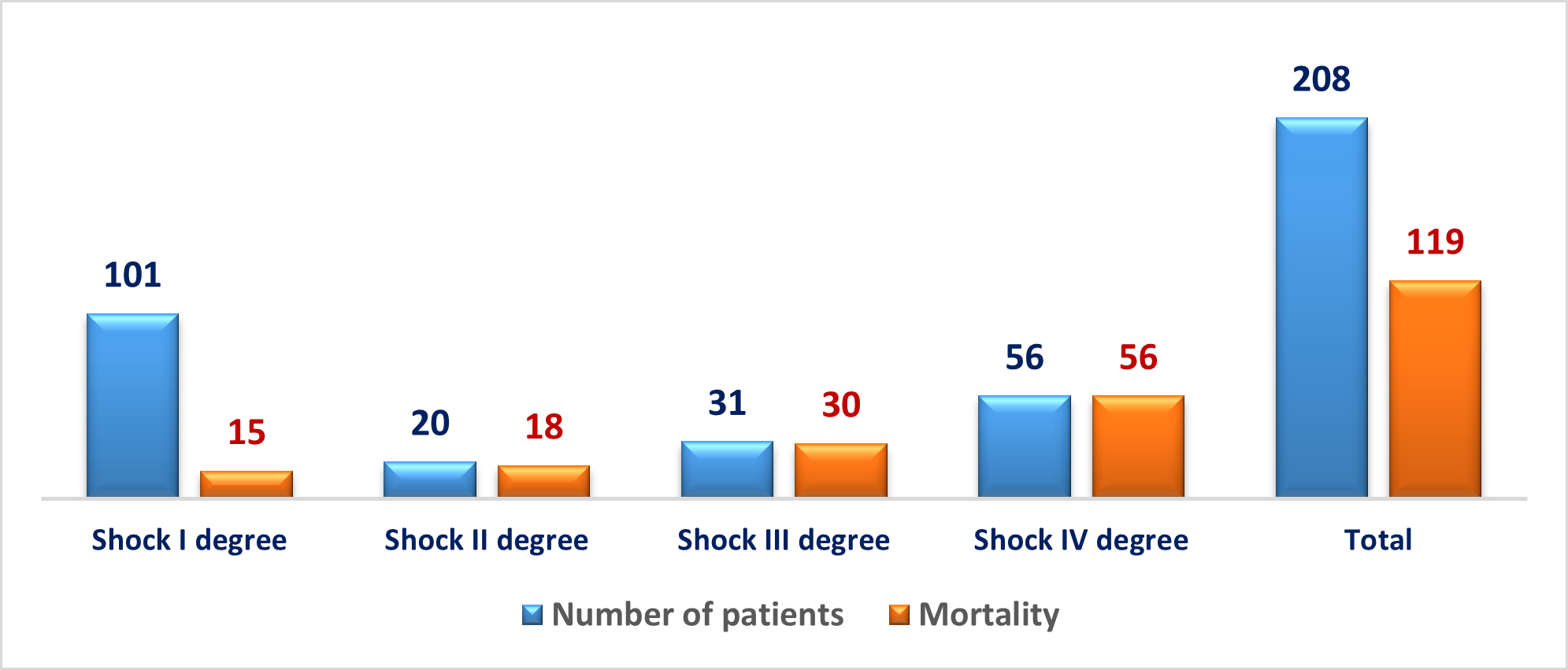
Attention should be paid to the fact that in the control group, even with the development of hemorrhagic shock of the 1st degree, there were cases of lethal outcome; with the development of hemorrhagic shock of II, III, and IV degrees, almost 100% mortality was noted (Figure 8).
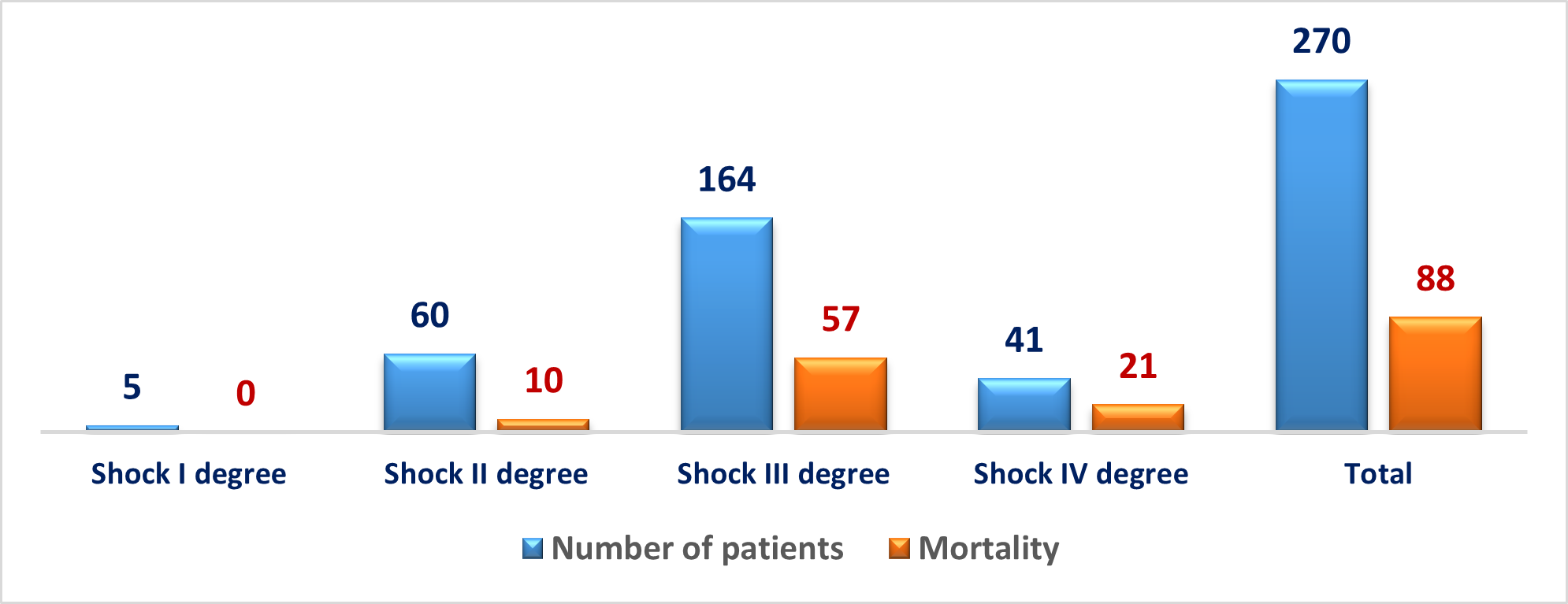
With the use of improved surgical tactics in the leading group, lethality significantly decreased, with no lethal outcome in the case of grade I hemorrhagic shock, and 49% of patients with grade IV shock survived (Figure 9).
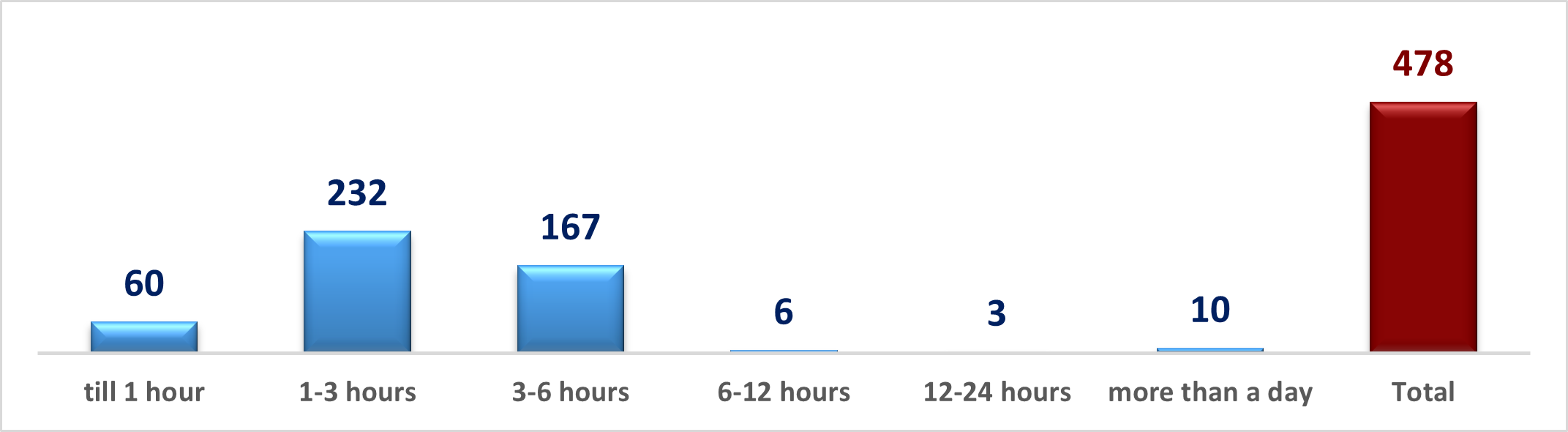
The following Figure 10 shows the terms of hospitalization of the victims in the hospital from the moment of injury. Most of the patients were hospitalized for 3 hours from the moment of injury (n = 292, 61.1%). Moreover, in the first hour after the injury – only 60 (12.55%) patients.
We also analyzed the frequency of damage to various anatomical areas of the body in victims with associated trauma (Figure 11). The largest group consisted of injuries to the head and limbs (62.0% and 58.9%, respectively), injuries to the chest organs – 40.5%, the spine – 27.2%, the pelvic bones, and urogenital organs – 22.9%, abdominal cavity – 21.2%.
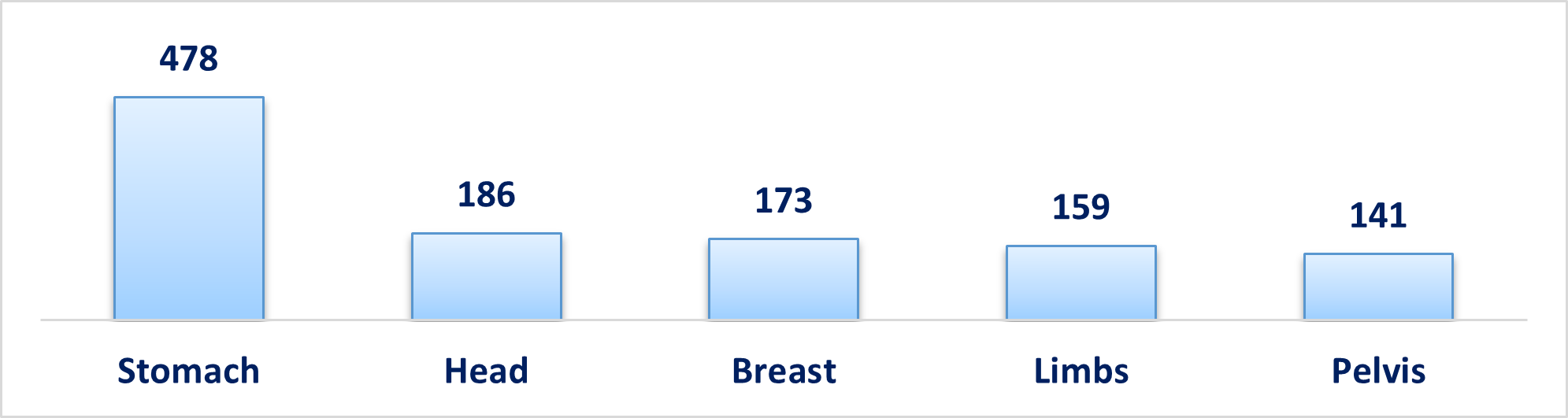
Among 478 patients with concomitant abdominal trauma, in 261 cases (54.6%), the predominant injury was abdominal trauma, in 131 cases (27.4%) – craniocerebral (TBI), in 60 patients (12.5%) – chest trauma and combined injuries were found in 26 (5.5%) cases.
Most often, abdominal injuries were associated with TBI and chest trauma (n = 271; 56.7% of cases).
It is important to note that in 94.1% of cases, injuries of two or more anatomical areas were detected.
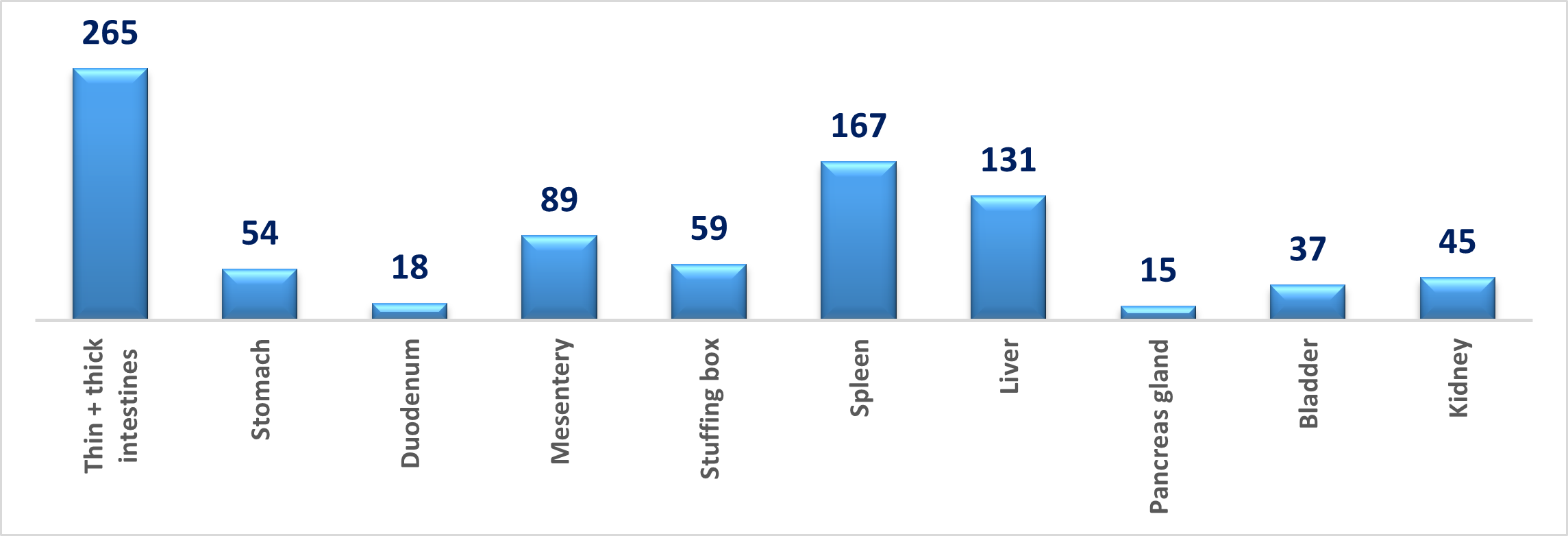
The total number of abdominal and retroperitoneal injuries detected in 478 patients is 880. Among the abdominal injuries, injuries of parenchymal organs were predominantly encountered (Figure 12).
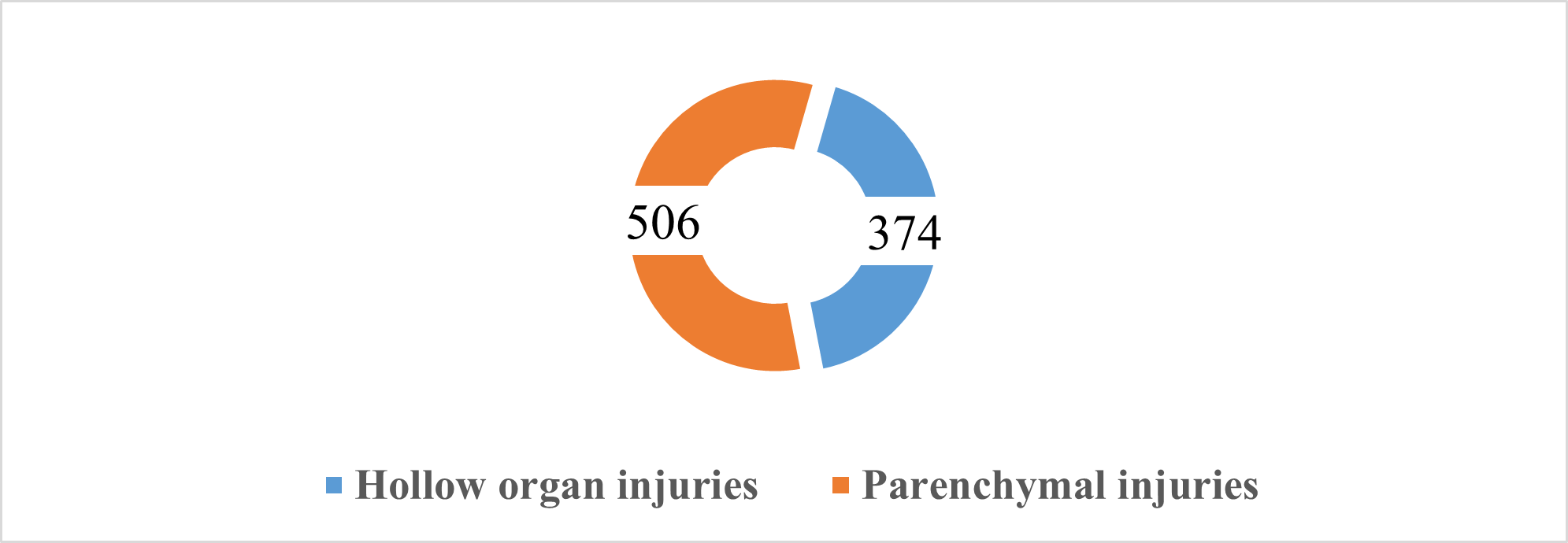
Damage to the parenchymal organs (506) of the abdominal cavity and retroperitoneal space prevailed over injuries to the hollow organs (374) of the abdominal cavity (Figure 13).
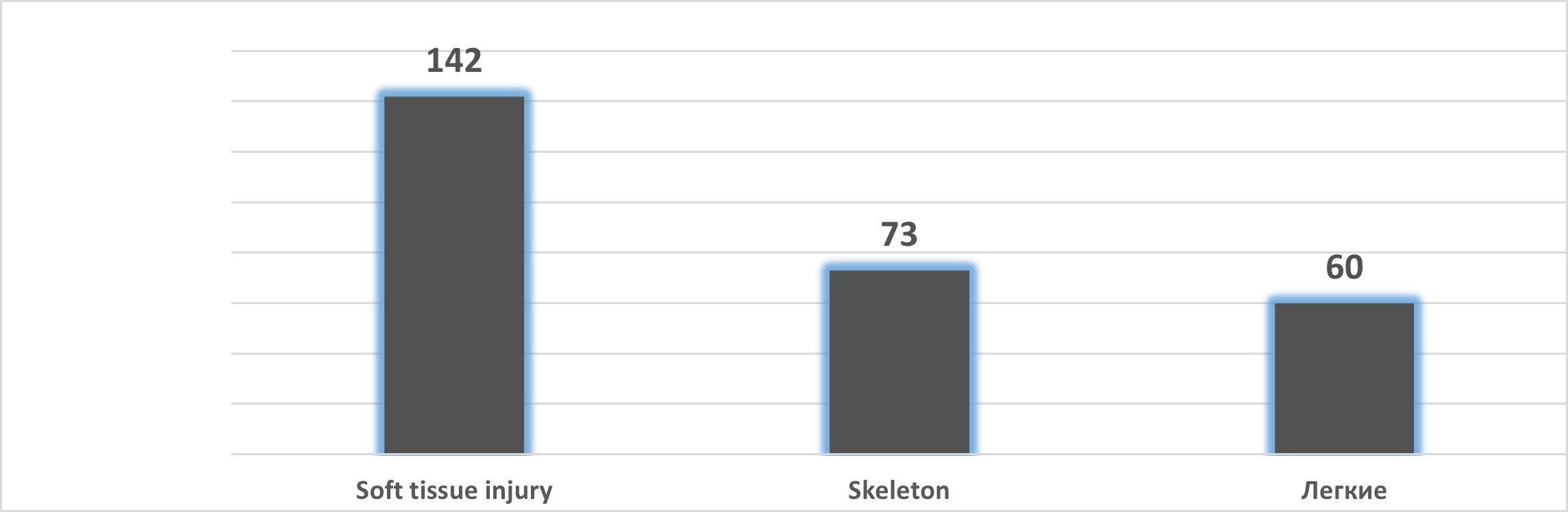
In addition, 275 patients had extra-abdominal injuries (Figure 14), which were characterized by damage to the skeleton, soft tissues and chest organs.
The intra-abdominal bleeding syndrome was observed in the case of damage to the parenchymal organs or blood vessels of the mesentery and omentum, retroperitoneal space. At the same time, changes in hemodynamics were characteristic, as well as a decrease in several hematological parameters (hemoglobin, hematocrit, the number of erythrocytes), oliguria, and leukocytosis with the ruptured spleen (in 167).
We adhere to the following treatment tactics: with a distinct clinic for intra-abdominal bleeding and acute peritonitis – emergency operation (in 232 patients). In the absence of confidence in the presence of intra-abdominal bleeding and peritonitis, together with anti-shock therapy, such diagnostic methods are performed as pleural puncture (in 31), laparocentesis (in 40), laparoscopy (in 127), R-graph: skull (in 51), pelvis (in 30), spine (in 37), retrograde cystography (in 15), ultrasound (in 201) and computed tomography (in 40 patients).
The most common combined abdominal trauma was damage to the parenchymal organs in combination with damage to the intestine, bladder, and kidney. It is considered that trauma to the liver, spleen, kidney, and extensive retroperitoneal hematomas were more often observed with damage to the chest, pelvis, and spine. On admission, symptoms of internal bleeding were noted in 250 (52.3%) patients and 48 (10.0%) patients with symptoms of peritonitis.
